The dentist-scientist career pathway in Africa: opportunities and obstacles
Article information
Abstract
The future of evidence-based dentistry in developing Africa heavily depends on a sustainable establishment of a vibrant dentist-scientist workforce. A dentist scientist is saddled with the responsibility of carrying out robust cutting edge research projects that are inspired by clinical experience. Currently, there are no pipelines in place to systematically train such dentists, neither are there programs in place to allow trained African dentists choose such a career pathway. A dentist-scientist is a person who studied oral, dental, maxillofacial (or craniofacial) diseases, prevention, and population sciences (obtaining a medical degrees such as bachelor of dental surgery [BDS] or BChD) alone; or in combination with other advanced degrees such as doctor of dental surgery (DDS)/doctor of philosophy (PhD) or BDS/PhD. This situation has resulted in overdependence of African clinical practice on research findings from technologically advanced Western countries and a decline in clinical research capacity building. The career path of a dentist-scientist should involve research along the spectrum of basic biomedical sciences, translational, clinical and public health sciences. There are several factors responsible for the ultra-low count of dentist-scientist in the heterogeneous African communities such as: poor biomedical research infrastructure; lack of funding; absence of structured dentist scientist career pathways; lack of personnel, inter alia. Hence, this review hopes to discuss the opportunities of setting up a dentist-scientist training pathway in Africa (as obtains in most developed world settings), identify opportunities and prospects of developing an African dentist-scientist workforce, and finally discuss the challenges involved.
Introduction
In the era of precision and personalized medicine, it is important for the African continent to equip itself with the requisite workforce that can handle and make sense of knowledge acquired from gene sequencing and genomics, proteomics, molecular imaging, bioinformatics and big data mining. This could improve the development of individualized therapies for diseases in Africans. Understandably, the biomedical research community in Africa has faced diverse internal and external bottlenecks over the years [1]. However, it is apparent that Africa is overdue for developing innovative research programs that systematically addresses its unique clinical conditions and disease burden. Even in the developed world, it has been reported, that there are disparities in biomedical research funding for ethnic minorities via government funding mechanism, and that increasing minority representation could promote better science [2]. Although, a huge burden of various diseases are found in Africa, it is unfortunate that there is still a very low amount of cutting edge health research originating from this region [3-5]. The lack of structured career paths within biomedical research institutions and medical schools is a major problem, albeit the problem facing biomedical research in Africa is multidimensional [6]. Not least, biomedical sciences curricula in most African medical schools do not inspire student to consider medical research as a career path; neither does it provide teaching in latest advances in the medical field [6].
The dental practitioner, academic and research communities in Africa need to contribute towards the establishment of a dentist-scientist workforce in Africa in order to address burden of dental diseases in Africa. In the era of precision medicine, novel discoveries in biomedical sciences is redefining the conduct of medical research and human health improvement [7]. However, the integrity of medical research in Africa depends heavily on the quality of data and knowledge of the health personnel involved in the data collection [8]. Despite these burgeoning body of relevant scientific knowledge emanating from biomedical research, only a few find their way into clinical application [9-11]; clinical problems are hardly translated into research projects [12]. Dentist-scientists are catalysts of translational research because they are able to bridge the gap between bedside and the laboratory while engaging research and clinical practice [13,14]. Having such a workforce in Africa would enhance the translation of basic research findings into clinical application, as well as developing clinically relevant research questions which are translated from the bedside into basic research [15-17]. Translational research is highly important to international health policies, development initiatives, and research funding [18]; and African governments need to create an enabling environment for translational research among its dental health care providers. A decline in medical/clinical research output and capacity has been found in Africa as a result of low counts of clinician-scientists [19]. Although the support of the pure scientist is needed to tackle dental research problems that emanate from clinical observation, dental practitioners should play a more important role in addressing these problems [20]. Over the years, medical science has experienced a shift from clinician-scientists focusing on a single problem to multidisciplinary team science focused at solving a complex problems of significance to the society at large [21].
The dentist-scientist workforce: status quo in Africa versus global scenario
With the ever changing clinical standard practice, biomedical research is deemed a powerful tool for addressing challenging in healthcare delivery [22]. Currently, innovative advances in biomedical sciences have paved a way for rapid diagnosis and treatment monitoring of diseases [23]. The increase in African health research publications mostly contributed by South Africa, Nigeria, and Kenya, does not necessarily equate an acceptable level of health research in the continent [24]. Overdependence of medical practice on scientific evidence from the developed world, which is obtained in most Africa countries, has not permitted the much desired advancement in the management of many diseases in the African setting [25]. Generally, expertise is deficient in evidence-based research, and research suggested this as a major attributable factor responsible for low research capacity in Africa. There are very few physician scientists in Africa and even rarer are dentist-scientists.
On the other hand, many developed economies have perfected ways to systematically incorporate science and research into dental practice. For example, the National Institute of Dental Research (NIDR) was established in America in 1948, and was highly instrumental in weaving science and technology research into the American dental schools, as well as applying science to inform the routine practice of oral healthcare [21]. After 50 years of remarkable expansion of the research and training portfolio of the NIDR, the name was changed to the National Institute of Dental and Craniofacial Research (NIDCR) in 1998 [21]. However, between 1999 and 2012, the number of grant applications awarded to dentistscientist is on the decline and there are also low numbers of new dentist-scientist investigators that apply for the National Institute of Health (NIH) early career programs [26]. As an emerging economy, there is a vibrant increase in the dental science research of Brazil and there seems to be a relative increase in dental research productivity (adjudged by h-index) of Brazil as compared to the United States [27].
A recently completed NIH study showed that growth of new doctor of philosophy (PhD) scientists who hold an NIH Research Project Grant surpassed that of physician-scientists [28]. Globally there is a continual decline in the physician-scientist workforce that hold the NIH Research Project Grant, but it follows an aging trend of established physician-scientists getting more NIH Research Project grants than early career physician-scientists [28]. This bottleneck that start-up dentist-scientists experience in technologically advanced societies would affect young and aspiring dentistscientists even more in Africa. In the sub-Saharan African region, there is lack of clinically trained dentalresearch scientists and minimal or no support for those existing [19]. To tackle the present precarious healthcare burdens appropriately, Africa need well-trained dentistscientists workforce to train future dental researcher and to lead research endeavours across the continent, and further afield.
Africa is a continent plagued by continuous and massive emigration of clinicians to technologically advanced and high income countries [29]. The current capacity of the dentist-scientists workforce in Africa is unknown as compared to an approximate 9,000 physician-scientists declared by the United States in 2012 with NIH research project grants [28]. Although there is a persistent decline in the physician-scientists workforce in developed countries [14,30,31], the paucity of dentally trained research scientists in Africa could present with retarded progress of evidence-based dentistry in Africa.
Innovative approaches to increasing the dentist-scientist workforce in Africa
1. Inclusion of research modules in undergraduate and post-graduate dental curriculum
Involving medical and dental trainees in translational clinical research all through medical school and during residency training has been proposed as a way of increasing the physician-scientist workforce [31]. In fact, in 2009, the Association of American Medical Colleges has recommended that clinical research training be accelerated and restructured in undergraduate and graduate medical education curricula in order to increase the population of physician-scientist workforce [32]. Thus various training programmes such as the doctor of medicine-PhD and doctor of dental surgery (DDS)-PhD pathway have been established in medical colleges in the United States to ensure continued production of physician-scientists [33]. In Africa, translational clinical research is yet to be incorporated into undergraduate curriculum of many medical schools [34]. Hence, there is an urgent need to re-evaluate and improve research capacity and training among dental trainees in Africa [35].
2. Government funded training programmes are needed
There is a dearth of dental scientist around the world and the situation is worse in developing countries. While most developed countries have taken a systematic approach to training and nurturing dental scientists, countries in Africa have yet to come up with any plans at all. In this section, we will review the dental scientist training pathways in the United States and propose a similar pathway in Africa.
The National Institute for Dental and Craniofacial Research is the primary institute at the NIH responsible for the training of dental scientists. These trainings are both intramural and extramural. The focus of this review will be on the extramural training where most of the dental scientists are produced.
DDS/PhD track: This program allows dental students to pursue a combined degree with emphasis on clinical and basic science research training. These students are enrolled in the DDS program and take courses in the first through fourth year of dental school. They are conferred with a DDS degree in the fourth year before starting their PhD program from the 5th to the 7th year. To ensure students are exposed to research experiences, most DDS/PhD students participate in the Student Undergraduate Research Training. After obtaining their DDS degrees, they are also given opportunities to practice for 1–2 days each week to ensure they maintain their clinical skills. Most of these individuals are also encouraged to pursue an advanced training in any of the dental specialty to increase their chances of a successful clinical and research faculty career. This program is usually funded through an institutional training grant from the NIH (T-90) or through direct individual fellowships (T-32) offered by the NIH to institutions based on merits and after peer-review. Of the 65 dental schools in the United States, only 18 of them offer DDS/PhD programs and currently enrol one to two students per year [36]. The low number of trainees is a major reason for the dearth in dental scientists. Nonetheless, it is obvious that there is a deliberate attempt to increase the dental scientist pool.
Additional strategies to increase this pool have been designed and implemented and these include: the dental scientist path to independence award (k99/R00) which is a 2 years mentored fellowship program for dentist with PhD and support for 3 years to become independent. There are also the K-awards (K01, K08, and K23) for young and middle level clinical faculty to become mentored in research for 2–3 years and support for 3 years as independent research faculty. Overall, these training mechanisms have enriched the dental scientist pool in the United States.
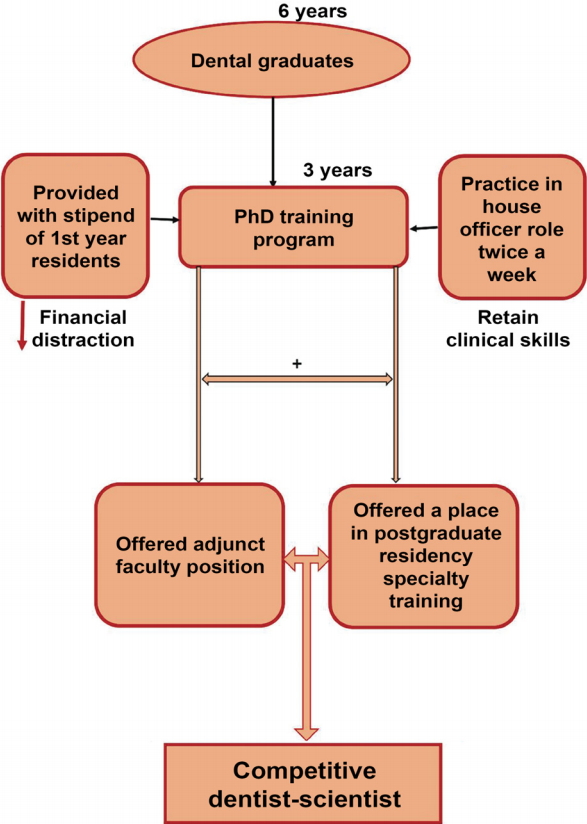
Is this possible in Africa? The answer is “yes.” Using the current dental training in Nigeria as an example, students can graduate after 6 years of dental school and commence their PhD training program immediately for 3 years. During the PhD program, they should be offered stipends commensurate with what first year residents earn. They should be allowed to practice for 2 days a week in a role similar to that of a house officer. This will help maintain their clinical skills. Upon completion of the PhD, they should be offered adjunct faculty positions as well as a place in postgraduate residency in any specialty of their choice in order for them to become competitive (Fig. 1). This program must be funded by the federal government and funds should be set aside in an endowment to ensure continuity and uninterrupted training.
How is this different from status quo? The proposed DDS/PhD program will be a game changer with multitudes of benefits to the dental scientist pool in Africa. Currently, individuals go through dental school for 6 years with no formal training in research, work as house officers for 1 year and serve the country for another year. They spend 2–3 years in private practice before starting postgraduate residency training. After 6 years of residency, they are employed as faculty with little or no research experience beside the minimal requirement before their fellowship is conferred. The majority of the faculty in dental schools in Nigeria went through this route and the result is evident on the level of dental research in the country. A few changed their training route and took additional postgraduate degrees like PhDs and master of public health and these individuals have distinguished themselves as successful scholars. It takes a minimum of 14 years to become a faculty under the current arrangement and a fixed 15 years to become a faculty through the dental scientist pathway. As it is in the United States, Nigeria and other African countries can start small by enrolling one or two trainees in three to five dental school each year into a dental scientist training program. In 10 years, there will be a critical mass of dental scientist and downstream effect on clinical basic, and translational research in dentistry will be unprecedented.
Improving the physician-scientist workforce in Africa: South African case example
1. National Health Scholars Programme
The South African Ministry of Health made a pronouncement to train 1,000 PhDs in health sciences through the National Health Scholars Programme over the next 10 years as a result of a steady decline in clinical research capacity in South Africa [37]. This is aimed at increasing the number of physician-scientists workforce in the country. The PhD Scholarships are awarded to health professionals for full-time doctoral research to be conducted in health sciences.
2. Clinician Researcher Programme: South African Medical Research Council
Another funding provided for dentist-scientists is the South African Medical Research Council–Clinician Researcher Programme, which is a full time PhD scholarship awarded to medical or dental graduates to conduct clinical or biomedical research. Beneficiaries of the scholarship are expected to spend at least 90% of their time conducting research and 10% on teaching and clinical activities.
3. Academic institution initiatives for physicianscientist training in South Africa
A few universities in South Africa have developed initiatives that would empower clinicians to pursue a physician-scientist career pathway. For example, the University of Witwatersrand-Carnegie PhD Programme provides 2-year funding for clinicians with MMed (master of medicine) or MChD (Medicinae ac Chirurgiae Doctoranda) to pursue a PhD [19]. Even though this program has enrolled up to 16 fellows, its sustainability is being threatened by the availability of local funders. Also, at the University of Cape Town, intercalated bachelor of science (med) honours/bachelor of medicine and bachelor of surgery (MBChB) and integrated MBChB/PhD tracks are available to undergraduate medical students at the end of the second year of the MBChB programme. This training pathway consists of a basic medical sciences research and coursework component; as well as a clinical training component, at the end of which an MBChB/PhD degree would be awarded [38]. Even though these programmes are available, for MBChB/PhD pathways, we are not aware of any such pathways for dentist-scientists.
Obstacles to training and retention of dentist-scientist in Africa
1. Infrastructure
Most countries in Africa have succeeded in training home bred physicians, who are equipped with baseline training in biomedical sciences. However, the high cost of biomedical infrastructure and laboratory set-up, has prevented many research and science enthusiasts from following a physician-scientist pathway [6].
2. Remuneration
Moreover, physicians who decided to follow the biomedical research pathway are poorly remunerated in comparison to their clinician counterpart [39]. This disparity in remuneration and poor training infrastructure makes the choice of becoming a physician- or dentist-scientist less attractive in the African setting. Most African doctors who are determined to pursue this career path often tend to go in search of such opportunities overseas.
3. Research funding
A vital benefit of training physician- or dentistscientists is their commitment towards preventive and improved therapeutic management of diseases [13]. However, funding is major factor to consider in sustaining a physician-scientist career [13,39]. Although Africa bears up to 90% of the global disease burden, it only has access to about 10% of global health research funding [40]. Governmental research funding for dentists and doctors who wish to become dentist-scientists is largely unavailable. In addition, most dentists are either inexperienced in research grant writing or are unwilling to pass through the rigor of securing research grants. In a dispensation when funding is being reduced due to austerity measures, the possibility of researchers losing their funding is high [39,41]. Therefore, the risk of losing such grants may be a deterrent to pursuing a dentist-scientist career in Africa.
4. Poor research networking
Weak intra-Africa networking in the area of research and funding has also hindered the effective use of limited resources for the production of maximal quality science and career opportunities in Africa; as well as incentives to retain the few available scientists [40]. Good network among African medical researchers is essential and can lead to better medical and dental research output in Africa. For example, an oral pathology research consortium known as the African Oral Pathology Research Consortium has worked as a leverage for multicentre oral cancer study in Nigeria [42]. Similarly, the African Craniofacial Anomalies Network has supported the capacity building and research in genomics and genetics of craniofacial anomalies through funding from the NIH and Wellcome Trust [43].
5. Lack of home-grown solution to African problems
The high burden of various diseases in Africa [44-46], demands a home-grown solution. There is a pressing need for a vibrant and capable physician and dentistscientist workforce in Africa, to participate in clinical translational research that will accelerate personalized scientific breakthroughs in the medical field. Currently, there are no support structures established in the medical training programmes of many African countries for doctors and dentists to transition into physician-scientist career track [6]; except for a few emerging programmes being initiated by academic institutions in South Africa, as alluded to earlier [19,38].
6. High demand for basic medical services
Owing to the high demand for basic medical services in Africa, and the need to support their respective families financially, most medical graduates in Africa are required to go into immediate employment as a service provider. Such compelling forces are most times beyond the power of the affected individuals and may contribute significantly to the unlikelihood of a medical or dental graduate pursuing a physician-scientist career pathway straight after finishing medical school. These factors militate against training clinician scientists at the postgraduate level; and medical graduates tend to opt for the more financially viable and faster enriching option. Not least, the high clinical workload mostly makes it very difficult for clinicians to secure dedicated time for research in a clinical position [13].
Conclusion
Investing in a structured dentist-scientist training programme in Africa would ensure an increase in dentistscientists workforce Africa and this would improve the systematic development of evidence based medicine for personalized medicine in the African continent. Hence, there is a pressing need for African governments to establish and support research and academic institutions that would provide better treatment for its populace. This would also enhance research capacity building for clinical research within the continent and reduce the overdependence on “first world” countries. This is possible, as we have seen as a good example in South Africa, albeit it is in its infancy. When there is a funding shortage, a physician-scientists tends to draw back to the more financially viable clinical discipline [41]. It is also recommended that medical training should involve a reasonable degree of biomedical research. The core undergraduate curriculum of most African universities need to provide science research development competencies in order to influence the decision of African trained dentists to be interested in a research career after their basic dental training. African hospitals should be supported by the government, and clinicians who need dedicated time to perform basic medical research should be funded in dentistry. We also recommend that the lengthy period required for basic dental degree, specialization and a PhD should be shortened to incentivize clinicians who are willing to pursue a dentist-scientist pathway in Africa. This can be accomplished by the establishment programs similar to that in South Africa. Collaborative linkages are also essential across Africa to foster a support system between countries. It is highly important for African governments to act strategically in developin, a talented stream of dentist-scientists workforce. This would create a conducive environment that develops, supports and retains existing physicianscientists; and attract back those in diaspora.
Acknowledgements
HAA would like to thank the South African Medical Research Council for a mid-career scientist research grant.
Notes
Funding
HAA is a recipient of a mid-career scientist research fellowship from the South African Medical Research Council. This work was also supported by NIDCR K99/R00 Grant DE022378-04 and Robert Wood Johnson Foundation Grant number 72429 to AB. The funders played no role in the design or interpretation of the paper or the decision to publish.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Authors’ contribution
HAA conceptualized, designed, prepared and critically revised the manuscript. AOA, OOS, and AB were involved in the design, preparation and critical intellectual revision of the paper. All authors read and approved the final manuscript submitted for publication.