Mediation effects of clinical practice stress between clinical education environment and satisfaction with clinical practice
Article information
Abstract
Purpose
The purpose of this study was to identify the possible correlations of ‘satisfaction with clinical practice (SA)’ with ‘clinical learning environment (EN)’ and ‘clinical practice stress (ST).’ We searched for the mediating effect of ‘clinical practice stress’ on ‘satisfaction with clinical practice’ when the clinical learning environment influences ‘satisfaction with clinical practice.’
Methods
This research investigated 208 medical and nursing students attending the school of medicine and nursing in Korea. The total number of nursing students was 135 (64.9%); 73 medical students participated (35.1%). We used the Korean-Undergraduate Clinical Education Environment in 24 questions for EN, ST scale in 24 questions, and SA scale in 10 questions. We performed measurement structural equation model analysis to identify a path of the model.
Results
Medical students had significantly higher levels of ST. EN had a significant negative correlation with ST and a significant positive correlation with SA. The ST had a significant negative correlation with SA. The results of the goodness of fit index have fulfilled the criteria of goodness of fit. There was a significant mediating effect of ST on SA when EN influences SA.
Conclusion
The clinical learning environment affected satisfaction with the clinical practice directly or indirectly mediated by clinical practice stress. Therefore, educational institutes should try to increase satisfaction with clinical practice by continuously monitoring and improving the clinical learning environment in addition to taking measures for decreasing the clinical practice stress.
Introduction
In general, the teacher, student, curriculum, and educational environment are considered significant education components. In clinical practice, students and supervisors, clinical practice programs, and clinical learning environments are the main factors for successful learning. For nursing students with a high level of satisfaction with clinical clerkship, autonomous and responsible learning occurred more [1,2]. However, when students had excessive stress and negative experiences, they had significant emotional hardship, including maladaptation, anxiety, and nervousness [3]. Particularly, those who experience high-stress levels during their clinical education tended to have lower satisfaction, performance, and nursing professionalism [4]. Medical students’ satisfaction with clinical practice has affected professional attitudes, career commitment, and retention [5,6]. Clinical practice was stressful because of having to deal with patients and unpredictable schedules in a new environment. The main stressors of trainees were context, communication, clinical scenario, and learning tasks [7].
The clinical learning environment affects learning, learners’ well-being, and satisfaction [8,9], thereby affecting learning ability, learning attitude, and career development [10]. Considering the significance of clinical practice in nursing and medical education, monitoring and improving the clinical learning environment is of great importance. Besides the regular curriculum, the hidden curriculum also has a considerable influence on learners. Therefore, hidden curriculum and environments should be considered one of the essential educational processes, and it is necessary to measure the educational environment and improve it. Thus, researchers have developed measurement tools for the clinical learning environment to analyze the educational environment [11-14].
However, the measurement tools had limitations in measuring some critical educational phenomena since many of them lack a theoretical basis, consider the clinical learning environment as a mere educational arena, and fail to acknowledge that it is a workplace as well [9,15]. They mainly measured either learning conditions in clinical placement or learning environments and supervision [13,14]. When measuring learning conditions, they assessed learning modeling, coaching, elaboration, research, and safety; and, when assessing learning environments and supervision, they measured the relationship with preceptors, educational environments, leadership style, and patient-related matters. To assess the clinical learning environments, learning opportunities, student participation, quality of supervision, workplace interaction pattern, and equal treatment extent also need to be factored in. The representative scale measuring those factors is the Undergraduate Clinical Education Environment Measure (UCEEM), which was developed to measure how undergraduate medical students perceive the educational climate in clinical environments and measure factors related to their learning and social interaction [16]. This scale has been verified in nursing and medical school's practice environment and can be used in both areas [17,18].
The factors that influenced one’s satisfaction with the clinical practice were practice workload, stress, emotional intelligence, and communication skills. The inter-professional relationships with fellow students, faculties, patients, and co-workers affected professional self-concept formation [16,19]. The primary factors that affect learners’ satisfaction with the clinical practice were the clinical learning environments as an external factor and clerkship stress as an internal factor. The stress of clerkship had negative correlations with students’ burnout, and satisfaction with a clerkship and resilience had a buffering effect on physical needs without mediating the psychological needs [20]. The stresses associated with clinical clerkship were inappropriate role modeling, a burden from practice workload, interpersonal conflicts, and conflicts with patients [21]. Students’ stress did not merely influence satisfaction with clerkship, but it also had adverse psychical and psychological effects on them. Therefore, medical and nursing schools need to consider stress management and provide more support to students during their clerkship [22].
The purpose of this study was to identify the level of ‘satisfaction with clinical practice’ in nursing and medical students who were doing their clinical practice in the one teaching hospital. Through this, we tried to find out the educational climate. We examined the possible correlations between ‘satisfaction with clinical practice (SA)’ and ‘clinical learning environments, (EN)’ and ‘clinical practice stress, (ST),’ respectively. Furthermore, we examined whether ST has a mediating effect on SA when the EN influences SA. Through this study, we would like to discuss what efforts are required by nursing and medical schools to improve learners’ satisfaction during clinical practice.
Methods
1. Participants
Two hundred and twenty-nine medical and nursing students attending the school of medicine and nursing, Konyang University, Daejeon, South Korea responded to the questionnaire, of which 208 were included in this study. The total number of nursing students was 135 (64.9%), of which the number of third-year students was 100 (48.1%), and fourth-year students were 35 (16.8%). The number of female students was 124 (91.85%), and male students were 11 (8.15%). Seventy-three medical students participated (35.1%), of which 29 (13.9%) were third-year students, 44 (21.2%) were a fourth-year students; with 24 (32.88%) female students and 49 (67.12%) male students. Nursing students had at least 3 to 8 weeks of clinical practice experience in a teaching hospital and should participate in orientation, ward round, core fundamental nursing skill learning, and case conference. Nursing professionals with a master’s degree or higher were in charge of clinical practice, and full-time faculty of a nursing college must direct at least 30% of the training course. Medical students had at least 24 to 56 weeks of clinical practice experience in a teaching hospital and must practice at least 36 hours per week. Faculties of medical college and residents as teachers were in charge of clinical practice. The subjects were nursing and medical students who participated in clinical practice in 2018–2019, and they agreed to participate after receiving information about the research contents before the survey. The Institutional Review Board of Tongmyung University approved this study (ethics consent no., TUIRB-2020-009).
2. Measurement tools
1) K-UCEEM
To measure the clinical learning environment (EN), we used Korean-UCEEM developed by Strand et al. [16] modified by Chun et al. [23] to adapt to the Korean context. This scale measures the educational climate and social interactions perceived by students. This scale consists of 24 questions based on five factors: workplace interaction pattern, equal treatment, quality of learning and supervision, clinical learning environment readiness, and learning opportunity. The examples of questions include “I feel included in the team of people who work here,” “Everyone is treated equally here regardless of gender,” and “I have adequate access to computers in this placement.” Each question was scored on a 5-point Likert scale, and a higher score indicated higher levels of positive perceptions of the EN. The Cronbach’s α was 0.939, and the sub-factors of the scale were from 0.769 to 0.880.
2) Clinical practice stress
To measure the clinical practice stress (ST), we used the scale developed by Beck and Sriavastava [21] modified by Kim and Lee [24]. This scale measures the level of stress perceived by students in clinical practice. It consists of 24 questions based on five factors: clinical learning environment, inappropriate role modeling, practice workload, interpersonal conflicts, and conflicts with patients. The examples of questions are “Space and facility for the clinical clerkship are lacking,” “The preceptors are not friendly and are indifferent towards the students,” and “The practice workload is too burdensome.” Each question was rated on a 5-point Likert scale, and a higher score indicated a higher ST level. The Cronbach’s α was 0.890, and the sub-factors of the scale were from 0.743 to 0.854.
3) Satisfaction with clinical practice
To measure the satisfaction with clinical practice (SA), we used four questions of Maastricht Clinical Teaching Questionnaire developed by Stalmeijer et al. [12] related to satisfaction with coaching and general satisfaction and five questions from the Manchester Clinical Placement Index developed by Dornan et al. [13] related to satisfaction with the clinical learning environment. The examples of questions are “Offered me sufficient opportunities to perform activities independently” and “This placement provided appropriate facilities.” Each question was scored on a 5-point Likert scale, and a higher score indicated higher levels of SA. The scales were translated and validated in Korean according to standard procedures before being used for nursing and medical students. The Cronbach’s α was 0.878, and the sub-factors of the scale were from 0.838 to 0.844.
3. Analysis
Data were analyzed using IBM SPSS ver. 21.0 (IBM Corp., Armonk, USA), AMOS ver. 22.0 (IBM Corp.), and frequency analysis to evaluate participants’ demographics. We calculated Cronbach’s α for reliability evaluation. Additionally, the relationships between variables were determined by using Pearson’s correlation coefficient analysis. We examined whether the observable variables in this study were appropriate for explaining the latent variables using structural equation modeling (SEM), then we performed “measurement model” analysis and “structural equation model” analysis to identify the path of the model. We used the bootstrapping method to analyze the mediation effect, sufficient for indirect effect analysis [25]. To evaluate the goodness of fit of the research model, we used χ2 (CMIN), root mean square residual (RMR), goodness of fit index (GFI), and root mean square error of approximation (RMSEA) for the absolute fit index, Tucker-Lewis index (TLI) and comparative fit index (CFI) for the incremental fit index.
Results
1. Differences in EN, ST, and SA between nursing and medical students
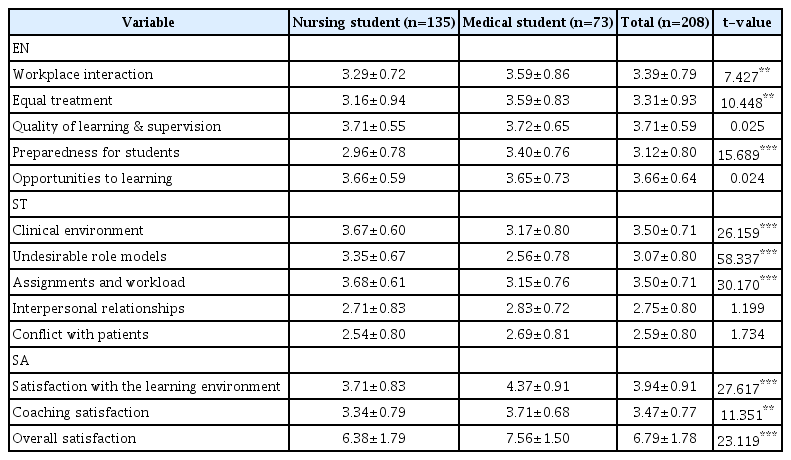
Table 1 shows the results of examining EN, ST, and SA perceived by students. In the sub-factors of EN, medical students perceived “workplace interaction” (t=7.427, p<0.01), “Equal treatment” (t=10.448, p<0.01), and “preparedness for students” (t=15.689, p<0.001) higher than nursing students. In the sub-factors of ST, nursing students perceived “uncomfortable clinical environment” (t=26.159, p<0.001), “undesirable role models” (t=58.337, p<0.001), and “assignments and workload” (t=30.170, p<0.001) higher than medical students. In the sub-factors of SA, medical students perceived “satisfaction with educational environments” (t=5.255, p<0.001), “satisfaction with coaching” (t=3.369, p<0.01), and “general satisfaction” (t=4.808, p<0.001) higher than nursing students.
2. Relationship between the variables
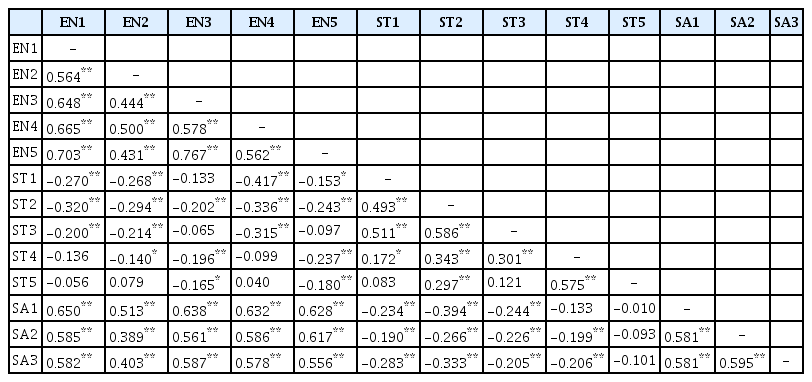
Results of correlation analysis between EN, ST, and SA were as follows. First, EN had a significant negative correlation with ST (r=0.322, p<0.01) and a significant positive correlation with SA (r=0.807, p<0.01). The ST had a significant negative correlation with SA (r=0.270, p<0.01). The results of correlation analysis among sub-factors of EN, ST, and SA are shown in Table 2.
3. Mediation effect of ST on the EN and the SA
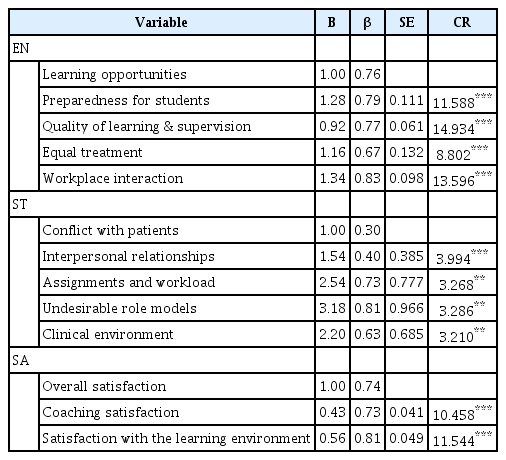
For the SEM analysis, we performed exploratory factor analysis to ensure that the observable variables used to measure the EN, ST, and SA could explain the latent variables. For parameter estimation, we used the maximum likelihood method. The results of goodness of fit index were as follows: χ2=133.841 (p<0.001, degrees of freedom [df]=59), χ2/df=2.268, RMR=0.037, GFI= 0.909, TLI=0.927, CFI=0.945, and RMSEA=0.078. The χ2 value was sensitive to sample size, that other GFI were considered together, then GFI, TLI, CFI were more than 0.90 [26,27], and RMSEA was less than 0.08 [28], fulfilled the criteria of goodness of fit. Since the factor loading (β) was from 0.30 to 0.83 (p<0.01) and met the criteria of more than absolute value for factor loading of 0.30, it was considered that the observable variables could appropriately explain each latent variable (Table 3). We analyzed the SEM to determine the path with which EN affects ST on SA.
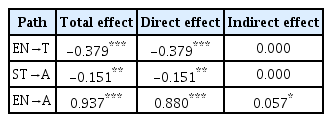
The goodness of fit index results were CMIN/DF=2.297 (p<0.001), RMR=0.039, GFI=0.914, TLI=0.925, CFI=0.946, and RMSEA=0.079, which showed appropriate goodness of fit (Fig. 1). The results identified as significant from path analysis are shown in Table 4. EN had a positive impact on SA (β=0.880, p<0.001). Otherwise, EN negatively affected SA (β=-0.151, p<0.01) through ST (β=-0.379, p<0.001). Lastly, we performed bias-corrected bootstrapping to verify the significance of the indirect effect of the EN through ST on SA (Table 4), and the indirect effect was 0.057 (p<0.05).
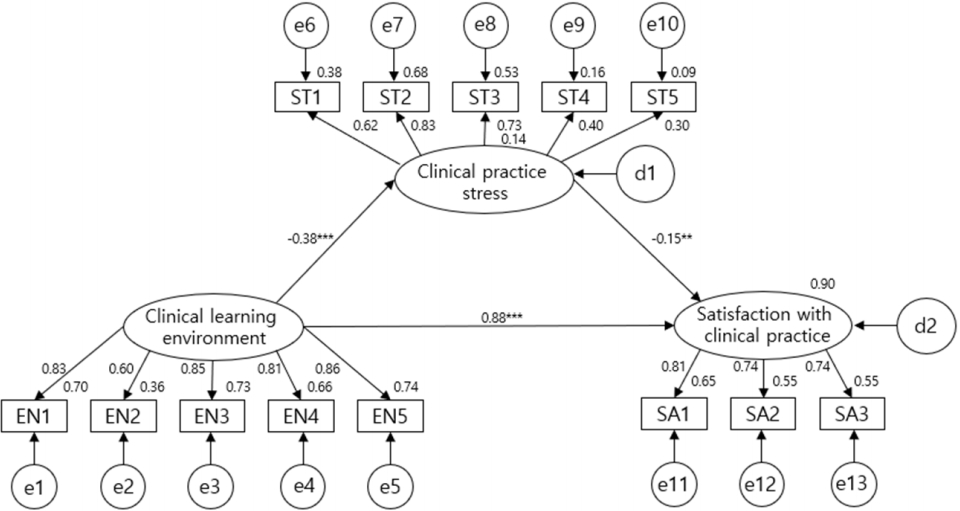
The Path Coefficients of the Final Model
EN1: Workplace interaction, EN2: Equal treatment, EN3: Quality of learning & supervision, EN4: Preparedness for students, EN5: Learning opportunities, ST1: Clinical environment, ST2: Undesirable role models, ST3: Assignments and workload, ST4: Interpersonal relationships, ST5: Conflict with patients, SA1: Satisfaction with the learning environment, SA2: Coaching satisfaction, SA3: Overall satisfaction. **p<0.01. ***p<0.001.
Discussion
This study examined EN, ST, and SA perceived by nursing and medical students and investigated EN and ST’s effects on SA. Also, the mediating effect of ST in EN affecting SA was verified.
Despite having practiced in the same hospital, nursing students had significantly lower SA than medical students and experienced more clinical practice stress. Such differences can be attributed to contents and methods of training and the leadership style of educators, and the type of coaching [29]. It may also be due to the difference in gender ratio in that the ratio of female students to nursing students is higher than that of medical students. These results are consistent with several series of studies suggesting that female students had a higher level of stress and fatigue and a lower level of satisfaction during clinical clerkship [30-34]. Due to the differences in the results, it is necessary to investigate if the differences in satisfaction levels between the two groups resulted from the differences in factors such as practice methods, jobs, education-related culture, and gender role differences. Although the practice was conducted in the one teaching hospital, the contents of clinical practice, duration of the training, and teaching style of training staff could differ in the nursing and medical college. Therefore, it is necessary to deal in-depth in subsequent studies on the differences in perceptions of students’ environment, stress, and satisfaction, and their causes.
EN was positively correlated with SA from correlation analysis between EN, ST, and SA. And there were negative correlations between EN and ST, and ST and SA. These results were consistent with that of previous studies [2,4,6,7]. In other words, students with more perception of stress had lower satisfaction. This study aimed to identify ST’s mediation effect on where the EN affected SA beyond a simple relationship between the variables. As a result, the mediation effect of ST was significant. The EN directly affected SA, and it had an indirect effect on SA. When students perceived the EN positively, they were less stressed and perceived higher SA. Therefore, educational institutes need to regularly inspect the clinical learning environment and monitor how cultural, physical, and human factors are perceived.
Additionally, they need to provide counseling and systematic support services to help the students reduce their stress and deal with interpersonal conflicts or conflicts with patients. Most of all, the learning environment factors identified in this study, such as workplace interaction, equal treatment, quality of learning and supervision, preparedness for students, and learning opportunities, should be improved. Moreover, the stress from inappropriate role modeling and practice workload should be reduced by means of the curriculum improvement and the faculty development programs. The consistent efforts to reduce the students’ stress include decreasing the discrepancies between students’ expectations and the real educational environments and solving the inconsistencies between the pre-clerkship education and the clinical practice [22].
In conclusion, with the current study on the differences in SA between nursing and medical students, and the relationship between EN and ST affecting the SA, we identified environmental improvement and stress reduction for improving students’ satisfaction with their clinical practice. The EN affected SA directly or indirectly mediated by ST. Because the current study was performed on clinical practice in a single teaching hospital, validation of multicenter follow-up study results is necessary. Furthermore, we suggest some research subjects identifying the reasons for the difference in satisfaction with clinical practice according to gender and the effects of consistent monitoring and measures for environmental education improvement on learners. We hope this study be useful in improving the quality of clinical clerkship.
Acknowledgements
None.
Notes
Funding
None.
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Author contributions
KHC: conception or design of the work and critical revision of the article; YSP: data analysis and drafting the article; MHK: first revision of the article; and all authors: final approval of the version to be published.