A simulation-based continuing professional development course for the first 5 minutes of cardiac arrest in the resource-limited local clinics
Article information
Abstract
Purpose
Using simulation in continuing professional development (CPD) courses for local practitioners is uncommon in Korea. The aim of our study was to evaluate the responses of the local practitioners for a simulation-based short CPD course.
Methods
Following the targeted needs assessment of local practitioners, we developed and implemented a 3-hour simulation-based CPD course for the first 5 minutes of cardiac arrest in the resource-limited local clinics. We evaluated the participant’s responses to the course using a questionnaire.
Results
During the 3-year implementation period, 115 practitioners participated in 10 courses, and 113 (98%) responded to the questionnaire. The overall course satisfaction (10-point scale) was very positive (10 in 93 [82.3%], 9 in 19 [16.8%], and 8 in 1 [0.8%]). The level (5-point scale) of recommendation to the others was also high (5 in 103 [91.2%] and 4 in 10 [8.8%]). Many participants positively commented on the authentic practical experience of the uncommon crisis in their contexts.
Conclusion
A simulation-based short CPD course for in-hospital cardiac arrest could provide an authentic practical experience for local practitioners working in resource-limited clinics.
Introduction
After graduating from medical school, all physicians must continue lifelong learning for their professional practice. Continuing professional development (CPD) includes all activities that physicians undertake, formally and informally, including continuing medical education (CME), in order to maintain, update, develop, and enhance their knowledge, skills, and attitudes in response to the needs of their patients [1]. Most learning in CPD is self-directed and based on physicians’ own learning needs. Effective CPD is characterized by three factors—needs assessment, appropriate learning activities, and follow-up on learning [2].
In 2014, with the foundation of the CME Accreditation and Evaluation Council, the Korean Medical Association (KMA) introduced mandatory credit and expanded the CME to the CPD [3]. In an analysis of 4,871 CPDs in Korea, lectures were adopted in 80.9%, and practical hands-on training course was only 0.4% [4]. Although a lecture is an efficient method for updating knowledge, other methods would be more effective in achieving specific learning objectives. Simulation provides safe and effective learning opportunities for all levels of learners to develop and maintain clinical skills [5]. A systematic review of simulation-based CPD demonstrated extensive variability in the design, delivery, and evaluation of simulation across specialties and the positive impact on individual and organizational performance [6]. Although simulation has been widely accepted as an education modality in undergraduate and graduate medical education, its use in CPD is uncommon in Korea.
The incidence of in-hospital cardiac arrest (IHCA) in local clinics has increased due to the increasing old age population and sedative use for endoscopy and cosmetic surgery in Korea [7]. The educational need for practical training on airway management and resuscitation skills of local practitioners has increased. To solve the problem and educational needs, we developed and implemented a simulation-based airway management and resuscitation training (ART) course for local practitioners.
Methods
1. Participants
The course participants were local practitioners working in cooperative clinics of a tertiary teaching hospital in Seoul. The medical referral center of the hospital has recruited participants via email in the second half of every year since 2017. The 12 practitioners participated in each course voluntarily.
2. Course development
Three emergency physicians with expertise in resuscitation and simulation education and an experienced simulation operations specialist (SOS) developed the course. The course development team developed a detailed consideration and application plan for the course according to the six-step approach of curriculum development [8] (Appendix 1).
In April 2016, the team conducted a meeting with four alumni practitioners to identify their educational needs and resource status in local clinics. After setting the goals and learning objectives, we aligned the educational strategies and assessment methods. Two pilot courses were performed for alumni practitioners of plastic surgery and internal medicine at the medical college-based simulation center. In the first half of 2017, in collaboration with the medical referral center, the team identified the educational needs of the cooperative clinics, and revised the simulation scenarios. After receiving three CPD credits from the KMA CME Accreditation and Evaluation Council, we implemented the first-year courses at the simulation center in the second half of 2017.
3. Course implementation
Before participating in the course, all practitioners voluntarily signed an informed consent after receiving a prior explanation about using the photographs, videos, and questionnaire along with a pledge of confidentiality for simulation training.
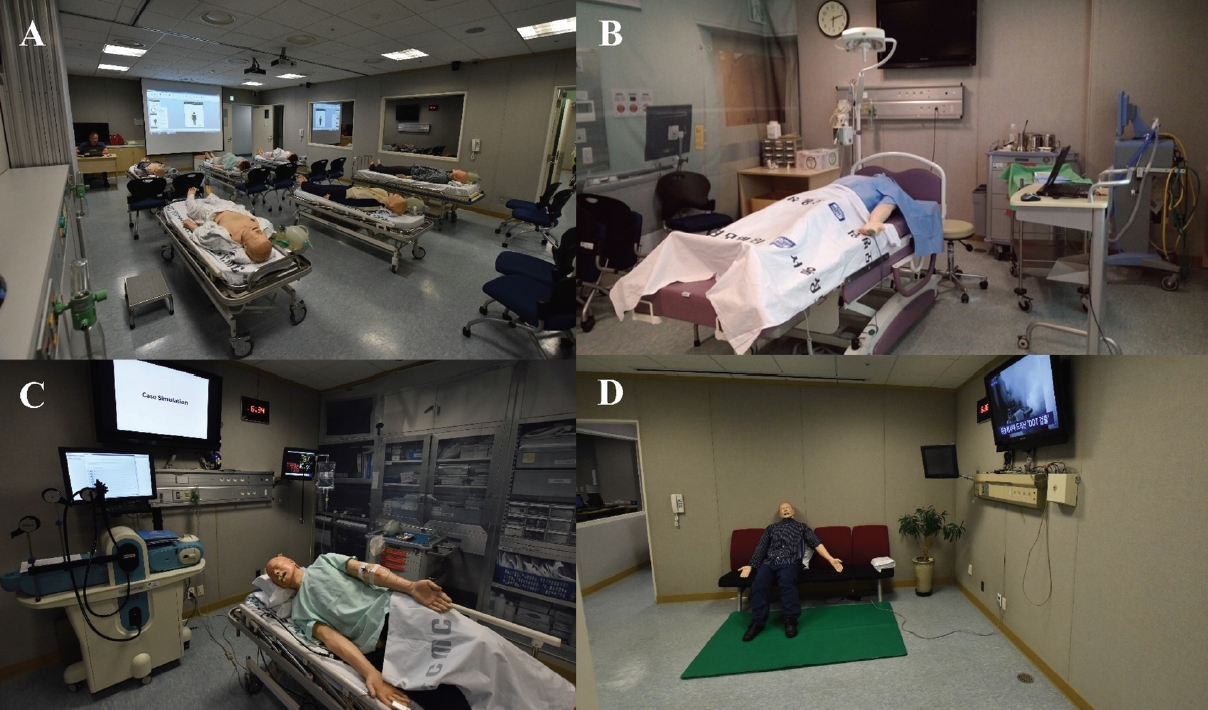
The ART course consisted of three sessions: (1) a brief lecture, (2) a hands-on practice workshop, and (3) a patient simulation (Table 1). Two emergency physicians and two SOSs delivered the course as the instructor team. In the lecture session, an instructor briefly reviewed 2015 Korean CPR Guidelines and the concept of crisis resource management. After a 10-minute break, two participants in a team participated in the hands-on practice workshop using various low-fidelity simulators. The participants practiced core airway management and resuscitation skills by watching the videos under the guidance and feedback of the instructors. Patient simulations were conducted using ALS simulator and SimMan (Laerdal, Stavanger, Norway) with two scenarios: (1) IHCA with initial shockable rhythm at the waiting area of the clinic; (2) IHCA with initial non-shockable rhythm at the endoscopy or minor surgery room. Fig. 1 shows the course room settings. In each simulation session, two instructors applied the rapid cycle deliberate practice method and stop-action debriefing [9]. The facilitator stopped the actions of the participants any time an error occurs and used a “pause and discuss/rewind” debriefing to allow the participants to redo a specific action after corrective feedback (Table 1).

The Time Schedule, Contents, Teaching and Learning Activities, and Assessment of the Airway Management and Resuscitation Training Course
4. Course evaluation
The course evaluation was conducted with a questionnaire immediately after the course. The questionnaire consisted of (1) a 10-point Likert scale evaluation for overall satisfaction; (2) a 5-point Likert scale evaluation for the training time, instructors, teaching methods, educational environment, recommendations to others; and (3) written comments.
Quantitative data were analyzed with descriptive statistics. Two investigators (Y.M.K. and S.A.L.) repeatedly read qualitative data independently and extracted major themes using the thematic analysis [10].
Results
1. General characteristics of participants
Ten courses were implemented during the 3-year period, and 115 practitioners participated in the courses. The participants’ sex was male (n=64) and female (n=51) and the median age (range) were 50 years (range, 35–73 years). Specialties were internal medicine (n=41), pediatrics (n=22), family medicine (n=11), otolaryngology (n=7), ophthalmology (n=7), orthopedics (n=7), obstetric (n=5), dermatology (n=5), urology (n=4), general surgery (n=3), rehabilitation (n=1), and neurology (n=1).
The clinics operated by the participants were classified as clinics among the types of medical institutions, with a small number (less than five) of medical personnel and limited equipment.
2. Course evaluation
Among the participants, 113 (98%) responded to the questionnaire. The overall satisfaction was very positive (10 in 93 [82.3%], 9 in 19 [16.8%], and 8 in 1 [0.8%]). The satisfaction level for the instructors was very positive (5 in 111 [98.2%] and 4 in 2 [1.8%]). For teaching and learning methods, responses were also positive (5 in 99 [87.6%] and 4 in 14 [12.4%]) and very positive (5 in 102 [90.3%] and 4 in 11 [9.7%]) for the learning environment. The level of recommendation to the others was also high (5 in 103 [91.2%] and 4 in 10 [8.8%]). Most participants evaluated that training time was optimal (n=112, 99.1%).
Most participants positively commented that they could have an authentic experience of the unusual crisis. They also mentioned repeated practice, connection to knowledge and practice, and an adequate proportion of instructors and learners as the good aspect of the course. Some participants wanted more diverse scenarios and team-based training with other staff members. In addition, some needed regular repeated training (Table 2).
Discussion
The ART course, a systematically designed simulation-based short CPD course for the first 5 minutes of IHCA, could provide authentic and practical learning experiences to local practitioners working at private clinics with limited resources. It would be an excellent example of how simulations can be effectively used for the CPD program on a specific topic requiring practical skill acquisition and maintenance for local practitioners.
Physicians’ CPD is not only a duty stipulated in the medical law but also an essential requirement for the self-development and self-regulation of medical professionals. It aims to promote and protect the public’s physical, mental, and social health. An effective CPD requires needs assessments, appropriate learning activities, and follow-up on learning [2]. Many practitioners have required authentic learning experiences to solve their workplace problems. Thus, simulation can be an effective teaching and learning method for CPD [5,6]. Many simulation-based CPD courses have been developed and implemented for procedural skill training for patient care. However, a simulation-based CPD course for local practitioners with limited resources has been limited in Korea.
The ART course was developed by faithfully following the guidelines for the judicious use of simulation technology in CME suggested by Curtis et al. [5]. According to local practitioners’ needs for the latest resuscitation guideline, we reviewed the current guidelines and then provided basic resuscitation skills training through deliberate practice. In consideration of the busy schedule of the local practitioners, we also have set realistic learning objectives so that the practitioners could gain confidence and a sense of achievement after the 3-hour short course and implemented it in the evening hour after the daytime practice. Furthermore, a step-by-step approach from low-fidelity simulation to more complex high-fidelity simulation has been applied to the participants unfamiliar with simulation modalities. In simulation-based training with experienced healthcare providers, preparing the same equipment and drugs in their workplace is essential. In the ART course, we identified equipment and drugs in local clinics during course development with local practitioners and developed scenarios using actual IHCA cases that happened at the clinics. These could be the strengths of the course.
Despite these strengths, there were some limitations to our course. First, we could not assess each participant’s performance with a validated tool due to the limited training time. Second, we only implemented two scenarios for patient simulation. It would fail to cover the educational needs of some participants. Third, although the simulation coordinators acted as the other personnel in the clinic during the simulation, the course participants were limited by physicians. Further efforts are required for the next steps, such as developing scenarios for more diverse situations and a team training course with other hospital staff members.
Acknowledgements
This is a collaborative project of the medical referral center of Seoul St. Mary’s Hospital and the START Center for Medical Simulation, College of Medicine, The Catholic University of Korea. We appreciate the faculty members of the medical referral center and the START center.
Notes
Funding: No financial support was received for this study.
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
Author contributions: Each author has made substantial contributions to the conception and design of the work (YMK, YMO, JHK, SAL), data collection (YMK, HJK, JEK, SAL), quality control of the data (CHC, YMK, YMO, JHK, SAL, JEK), interpretation of the results (CHC, YMK, YMO, JHK, JEK, SAL), and participated in drafting or revising the manuscript (CHC, YMK, YMO, JHK, JEK, SAL). Furthermore, all authors agreed to accept equal responsibility for the accuracy of the content of the manuscript and approved the manuscript to be submitted.