Scoping review: exploring residents’ views of supervisor entrustment and its effect on learning and professional development
Article information
Abstract
This scoping review aimed to systematically explore the complex and nuanced perceptions of residents entrusted with significant responsibilities by their supervisors in the clinical context. We conducted a comprehensive search strategy targeting six major electronic databases. Data were extracted using the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist and a scoping review protocol. Resident perceptions regarding entrustment and its impact on learning and professional development were categorized. This review elucidated the role of supervisor entrustment in shaping residents’ clinical performance, notably influencing autonomy, self-confidence, responsibility for patients, learning needs and goals, uncertainty management, and professional identity formation. Residents identified factors that promote and hinder performance and entrustment development resulting from supervisor entrustment and distinguished between appropriate supervision and over- or under-supervision. Our review suggests that residents’ perceptions of supervisor entrustment, as bestowed by supervisors, serves as a catalyst for enhancing autonomy, thereby exerting a significant influence on clinical performance, and fostering the development of a professional identity. However, residents’ views on appropriate supervision differ in some ways from supervisors’ perspectives. Further research is needed to bridge the gap between residents’ expectations of autonomy and what they are given, and to explore the intricate relationship between autonomy and entrustment.
Introduction
According to the Oxford dictionary [1], “entrust” is defined as “to make someone responsible for doing something or taking care of someone,” and “entrustment” is defined as “the act of entrusting.” In medical education, the process of entrustment by supervisors commences with the allocation of responsibilities pertaining to fundamental tasks, including interviews with patients, and gradually progresses toward granting trainees the autonomy to engage in independent medical practice [2]. A framework encompassing five levels of supervision has been proposed for pragmatic considerations. The entrustment is task-specific and contractual, wherein the clinical supervisor assumes accountability while the trainee executes the assigned tasks at a proficiency level commensurate with their individual competence.
Faculty members have diligently endeavored to determine the appropriate extent of entrusted responsibility to be bestowed upon residents with the objective of progressively increasing their autonomy while upholding patient safety [2-9]. Numerous systematic reviews have been conducted comprehensively investigating the multiple factors that influence supervisors’ decision-making processes when entrusting residents with specific tasks [10-13]. Hauer et al. [10] described this decision-making process in terms of five factors affecting supervisor trust: “supervisor,” “trainee,” “context,” “task,” and “supervisortrainee relationship.” According to Hauer et al. [11], these five factors, their interactions, and the various barriers and accelerators of each component explain the supervisor entrustment process. An entrustment decision-making process framework proposed by Holzhausen et al. [12] suggests that the supervisor considers contextual factors, resident character, and task-specific characteristics when determining the degree of supervision. Ten Cate and Chen [13] summarized that agency, reliability, integrity, capability, and humility are trainee factors that influence entrustment decisions.
Despite extensive research on the process of entrustment, some studies have shown that there is still a mismatch between what residents seek and what they are given, limiting resident education [14-17]. Furthermore, researchers have described the disparities in perceptions regarding levels of entrustment between residents and faculty members as potential impediments to the ultimate objective of resident training: the development of an “independent physician capable of providing autonomous care” [16,17]. To solve these problems, scholars have posited that supervisors must navigate a delicate balance by determining the optimal level of entrustment that fulfilled trainees’ educational requirements while simultaneously upholding patient safety [18,19]. Numerous literature reviews have addressed the concept of entrustment decisions from a supervisor’s viewpoint.
Understanding residents’ perceptions of the entrustment decisions made by supervisors and the impact of these decisions on their learning and competency development can provide critical information for improving resident training. Currently, there are few literature reviews pertaining to research examining residents’ perceptions of entrustment and the influence of these perceptions on their professional development. Therefore, this study aimed to conduct a comprehensive scoping review of the pertinent literature, meticulously delving into the nuanced and intricate perceptions of residents when entrusted with substantial responsibilities by their supervisors.
The authors of this scoping review aimed to (1) examine residents’ perceptions and sentiments pertaining to supervisor entrustment and (2) explore the interrelationship between these perceptions and their impact on professional development. The specific research question was, “What thoughts/perception do residents have when entrusted by supervisors, and how do these thoughts influence residents’ learning and the development of their competence?”
Methods
The term “entrustment” in this study was defined as the process of assigning responsibility for patient care. The extent of supervision varies from direct oversight to granting complete autonomy. The scope of this study encompassed research that explicitly indicated the level of entrustment (direct, indirect, or no supervision), as well as studies from which the level of entrustment could be inferred based on available data. Our scoping review applied the protocol methodology by Arksey and O’Malley [20].
1. Inclusion and exclusion criteria
The inclusion and exclusion criteria for this study were defined as follows:
1) Inclusion criteria
a. The selected studies focused on resident perceptions of supervisor entrustment, encompassing residents’ perspectives after assuming responsibility for patient care at entrustment levels 2–5 [2].
b. We limited the studies to those conducted in authentic clinical settings, and excluded simulated environments, virtual reality simulations, and simulation laboratories.
c. The publication period for the eligible studies ranged from 2012 to 2022.
d. Only studies published in the English language were considered for inclusion.
e. The selected papers were required to either explicitly describe the level of entrustment (e.g., direct supervision, indirect supervision, or unsupervised practice) or provide data from which the implied entrustment level could be inferred, even if not explicitly stated.
f. The inclusion criteria encompassed a wide range of research methodologies, including quantitative, qualitative, and mixed-methods studies.
2) Exclusion criteria
a. Studies that solely focused on students, supervisors, faculty members, or other healthcare professionals who were not residents, such as nurses, pharmacists, and dentists, were excluded.
b. Additionally, even studies that included residents were excluded if the results did not adequately differentiate the responses of residents from those of other participants (e.g., faculty).
c. Studies with resident assessments that were predominantly carried out by individuals other than supervisors were excluded from the analysis.
d. General opinions or commentary without the inclusion of actual trials were excluded.
e. We also excluded studies that primarily focused on the effects or outcomes attributed to factors other than supervisors’ entrustment.
f. Studies that focused on topics unrelated to residents’ perceptions were excluded.
2. Identifying the relevant studies
The search focused on studies that explored resident perspectives following supervisor entrustment. We collaborated to develop a comprehensive search strategy to facilitate data retrieval. Our search query incorporated medical subject headings (e.g., MeSH, EMTREE), relevant keywords in the title and/or abstract, terms related to entrustment and its subdomains (e.g., trust and entrust), and specific terms related to residents (e.g., trainee and learner). We conducted searches across six electronic databases: PubMed, Embase, Web of Science, Scopus, ERIC, and the Cochrane Library, and complemented our data collection with manual searches. The scoping review included peer-reviewed publications, such as primary literature, review editorials, and commentary/opinion pieces, but did not include conference proceedings. The search encompassed publications from January 1, 2012, to November 4, 2022. A complete version of the search strategy can be found in Supplement 1.
3. Selecting the studies to be included
All data were imported and managed using the EndNote software ver. 20.0 (Clarivate, Philadelphia, USA). The study selection process consisted of the following five steps. First, three reviewers (S.H.S., H.S.K., and Y.M.L.) dedicated time to thoroughly understanding the research questions. Second, to increase consistency among reviewers, all researchers did the following: reviewed 130 identical publications (15% of all articles), discussed the results, adjusted the review and data extraction manuals, and then began the review. All reviewers independently assessed potentially relevant publications and sequentially evaluated titles and abstracts against inclusion and exclusion criteria. Disagreements about selected articles were resolved by iteratively comparing our lists of included and excluded studies and engaging in discussions to reach consensus. In the third step, the researchers independently evaluated the titles and abstracts of the remaining articles to determine their eligibility for inclusion, adhering to the predetermined criteria. In the fourth step, they discussed discrepancies in the selected papers and resolved them through mutual agreement. Finally, full-text screening was conducted using the established inclusion and exclusion criteria.
4. Charting the data
Data extraction from all full-text articles was conducted by the reviewers (S.H.S., H.S.K.) using the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) checklist and the scoping review protocol [21]. The two reviewers independently charted the data, discussed the results, reconciled any discrepancies, and continuously updated the data-charting form iteratively. During this collaborative discussion, efforts were made to ensure the uniformity and clarity of the data extraction process. Additionally, the extracted data were supplemented with pertinent details to enhance comprehensibility. Through iterative deliberation, the results were categorized based on the identified themes and key findings.
5. Collating, summarizing, and reporting results
Through comprehensive data analysis, a synthesis of resident perceptions regarding supervisor entrustment was undertaken, specifically exploring the impact on residents’ learning and professional development. We counted the number of studies included in the review that potentially met our inclusion criteria and noted the number of studies that had been missed by our search. The database search yielded 1,549 articles, while the manual search yielded an additional 26. The removal of duplicates resulted in 847 articles. After screening the titles and abstracts, 784 records were excluded and 63 articles underwent full-text review. Of these, 47 papers were excluded, and 16 were finally selected. Fig. 1 shows the PRISMA flowchart for item identification. The overall characteristics of the reviewed articles are summarized in Table 1. Reviewers extracted data on article characteristics, including authors, title, country of origin, year of publication, methodology used in the study, participant specialty (resident), entrustment level, and the workplace where entrustment took place. We grouped the findings they analyzed, summarized entrustment levels and residents’ perceptions of supervisor entrustment, and synthesized the results.
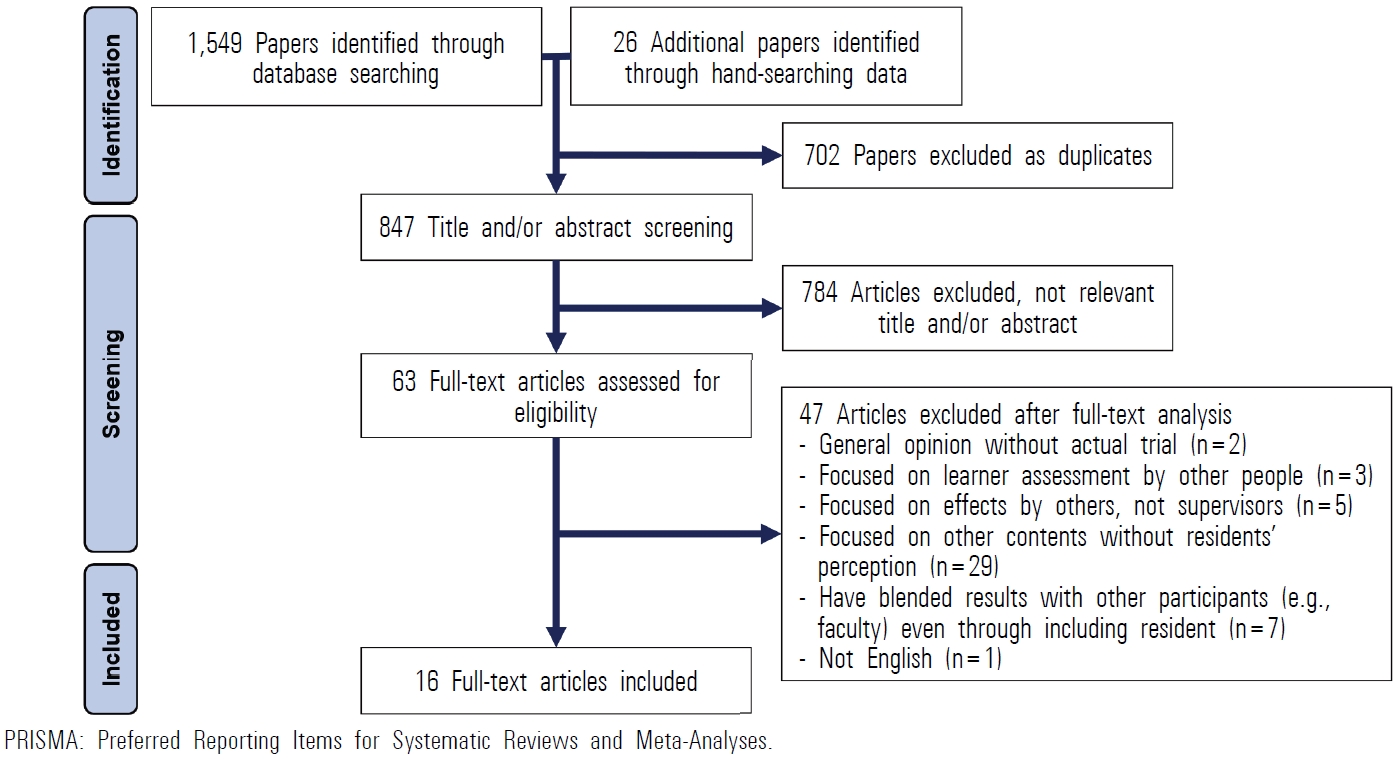
The PRISMA Flow Diagram for Article Identification
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Results
The scoping review identified three major themes. First, supervisor entrustment significantly influenced resident performance, including autonomy, self-confidence, responsibility for patient care, changing learning needs and goals, ability to manage uncertainty, and professional identity formation. Second, the residents identified both promoting and hindering factors affecting their performance development through supervisor entrustment. Table 2 shows the key findings of the analyzed literature regarding resident performances influenced by supervisor entrustment and the various factors that affect residents’ entrustment development.
1. Effects of supervisor entrustment on resident performance
1) Autonomy
Residents perceived that their supervisor’s entrustment influenced the development of their autonomy. Specifically, the level of supervision, resident competency, supervisor personality, atmosphere of practice, and supervision style were identified as key determinants affecting the progression of resident autonomy. Moreover, fostering autonomy among residents cultivates a heightened sense of responsibility toward patients and boosts self-confidence, consequently facilitating the ongoing progression of resident autonomy [3,22-28]. Sawatsky et al. [3] examined the development of professional identity and the interplay between autonomy and supervision through interviews with 23 residents of internal medicine. Results revealed that resident autonomy evolved when residents perceived the level of supervision as appropriate, prompting them to strive for higher levels of entrustment [3]. Furthermore, residents reported a sense of autonomy when they performed their assigned tasks well and experienced development in their entrustment level [24-26]. However, both over- and under-supervision were found to have negative effects on resident autonomy [22-24,26,28].
2) Self-confidence
Although several factors influence self-confidence, including autonomy and self-regulated learning, supervisor entrustment has been identified as an important factor. This includes the presence or absence of a supervisor and the characteristics and teaching approach of the supervisor during entrustment [3,22,23,25,26,29,30]. Perceived self-confidence varies with the level of supervision. At low levels of entrustment, self-confidence tends to be low as well. However, repetitive training under intensive and direct supervision has been demonstrated to enhance autonomy, resulting in increased self-confidence [29]. In the operating room, residents experienced an enhanced sense of self-confidence when attending physicians valued their opinions, maintained a relaxed demeanor, and provided specific learning objectives and constructive feedback. In contrast, residents reported decreased self-confidence with over-supervision [26].
3) Responsibility for patient
The supervisors’ entrustment has been found to contribute significantly to residents’ heightened responsibility for their patients [3,25,27]. A multi-institutional study provided evidence that trainees exhibit a comparable level of responsibility toward patients as attending physicians. Greater levels of independence among trainees are associated with a concomitant increase in their sense of responsibility toward patients [27]. Similarly, a study of internal medicine residents found a direct correlation between high levels of entrustment and an accompanying increase in autonomy, with a noticeable increase in residents’ sense of responsibility in the process [3]. Residents from various specialties acknowledged the inherent conflict between the need for supervision and their responsibility to deliver timely and accurate care. In such situations, residents perceived their supervisors as a safety net, enabling them to make errors without compromising patient well-being [25].
4) Changing learning needs and goals
As the level of entrustment evolves over time, the learning needs and goals of residents also change [22,25,28,31,32]. When residents perceived an increase in their competence, expanded their level of entrustment, or recognized their supervisors’ preferences, their learning needs shifted. Sheu et al. revealed a distinct shift in residents’ preferences regarding the level of supervision throughout their training. Residents in the early stages favored close supervision during patient encounters, but as their skills developed and they gained more experience, their inclination shifted toward autonomy, needing only indirect supervision or independent practice [22]. When deliberately challenging themselves by exceeding their entrustment levels, residents considered their development in terms of their competence [25]. The intention of residents to pursue specific learning goals in the case of an attending surgeon is influenced by their perception of the surgeon’s willingness to teach in the operating room [31]. In addition, residents exhibited a dual capacity in determining their learning needs and adapting their learning approaches to align with the teaching styles of their supervisors. Apramian et al. [32] discovered that surgical residents acquired knowledge of their supervisors’ preferences, procedural techniques, and underlying principles and subsequently made appropriate adjustments to their learning goals.
In contrast, when there was a significant difference between the level of autonomy expected by a resident and that provided by a supervisor, it reduced motivation for learning [22,28]. According to the research by LaDonna et al. [28], prolonged direct observation resulted in emotional distress among residents and prompted a shift from a patient-centered approach to a performance-centered care approach. This shift resulted in a decline in residents’ motivation to learn and led them to question the authenticity of their training [28].
5) Managing uncertainty
Residents’ approaches to managing and confronting uncertainty vary according to their level of entrusted responsibility [33]. Bochatay and Bajwa [33] found that residents of Switzerland were granted a higher level of entrustment (indirect supervision) than their counterparts in the United States. Swiss residents perceived themselves as autonomous practitioners and, when faced with uncertainty, were inclined to resolve it independently rather than seek guidance from their supervisors. They reported that these experiences contributed to the development of autonomy. Conversely, in the United States, where residents received direct supervision, when faced with uncertainty, they actively acknowledged it and sought guidance from their supervisors by asking questions. While this behavior was seen as conducive to learning, residents felt that their role was more akin to that of students.
6) Professional identity formation
Residents perceived that the level of supervisor entrustment significantly influenced the formation of their professional identity and their role as physicians [3,23]. The development of professional identity is influenced by various factors, including autonomy, self-confidence, patient safety, teaching style, relationships with supervisors, and the overall environment. One study utilizing Bandura’s Social Cognitive Theory demonstrated that as the level of entrustment increased, residents experienced a corresponding increase in autonomy, enhanced self-confidence, and a greater sense of responsibility toward patients, ultimately fostering further development of autonomy [3]. Residents’ professional identities are formed through this cyclical process [23]. When supervisors provided competency-appropriate tasks, made themselves available, facilitated debriefing, offered supportive feedback, and established mutual trust with residents, the residents were able to establish a clear role within the team [3]. However, residents perceive that over-supervision deprives them of the opportunity to actively participate in patient care, hindering the development of their professional identities [3,23]. Conversely, when residents experienced under-supervision, they expressed concerns about patient safety, which had a detrimental impact on their professional identity formation [3,23].
2. Promoting or hindering factors on resident’s entrustment development
Several studies have reported factors that promote or hinder resident entrustment development as perceived by study participants [18,25,26,34]. Promoting factors included: (1) residents feeling comfortable with their current level of supervision, (2) supervisors providing constructive feedback, (3) duration of continuous work under the same supervisor, and (4) supervisors demonstrating a positive attitude. Residents perceived their supervisors as a safety net when the level of supervision was appropriate, enabling them to make errors without compromising patient well-being [25]. Residents were more likely to extend themselves to higher-level referrals when patient safety was ensured, they had sufficient confidence in their abilities, and they had previously demonstrated competency under supervision [25]. A multicenter study reported that surgical residents recognized that immediate goal-directed feedback improved their entrustment development [18]. Residents also reported that consistently participating in surgeries with the same faculty over long periods strengthened entrustment as supervisors tailored their training to individual residents. In addition, another study showed surgical residents felt that entrustment development increased when supervisors displayed characteristics such as composure, patience, and receptivity to ideas and provided sufficient communication before and after surgery [26].
In contrast, several factors that hindered the development of entrustment were: (1) a lack of learning opportunities, (2) unclear teaching objectives, (3) neglect or micromanagement, and (4) supervisors’ negative attitudes [18,26,34]. The limited availability of new surgical instruments resulted in a lack of experience and served as a significant obstacle to achieving level 2 entrustment [34]. Sandhu et al. [18] discovered that residents expressed uncertainty because of unclear feedback from supervisors and ambiguous resident training guidelines in the operating room, which impeded the development of entrustment. Rivard et al. [26] revealed that treating residents as mere observers and excessive micromanagement in the operating room restricted the progress of entrustment. Additionally, rude, condescending behavior, impatience, and a lack of communication regarding clinical reasoning or decision-making were identified as factors that hindered the development of entrustment. These factors are simplified and shown in Fig. 2.
3. What is appropriate supervision for a resident?
Factors such as competency-appropriate tasks, mutual trust between supervisors and trainees, feedback from supervisors, and an environment that respects resident autonomy all influenced whether residents perceived the level of supervision as appropriate [3,18,22-24,26]. Residents deemed supervision as appropriate when the assigned tasks are aligned with their level of difficulty, provide continuity, and allow for autonomy while ensuring patient safety [3,22]. They also stated that supervision was appropriate when supervisors demonstrated an accepting attitude, shared learning goals, and effectively communicated about patient care [3,22,24]. Additionally, residents perceived supervision as adequate when supervisors actively supported them and provided clear feedback, especially in challenging patient situations, affording the trainee sufficient autonomy to work for the benefit of the patient [18,23,26].
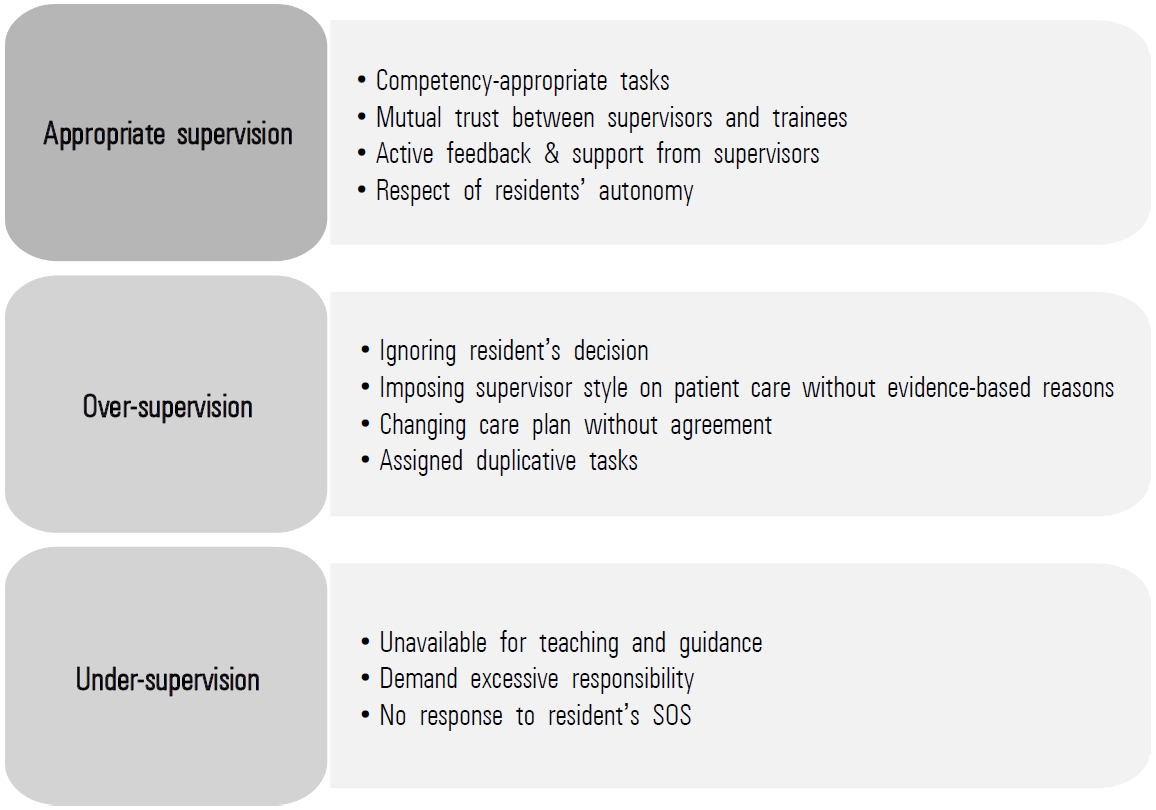
While an appropriate level of supervision prompts residents to strive for higher levels of entrustment, both over- and under-supervision have been shown to have a negative impact on the development of resident performance [22-24,26,28]. Both under- and over-supervision were identified as factors that instilled fear in residents regarding the safety of their patients [23]. Autonomy, self-confidence, responsibility for patients, and ultimately professional identity were negatively affected by either over- or under-supervision. Residents felt that supervisors over-supervised when they excessively interfered with their decisions during entrustment, imposed personal styles on patient care without providing evidence-based reasons, changed care plans unilaterally, or assigned duplicative tasks [22-24,28]. On the other hand, residents thought that supervisors under-supervised them when supervisors were unavailable for teaching and guidance and demanded more patient care responsibilities than residents expected, and when residents could not ask for help [22,23].
However, for certain tasks, the residents expressed a consistent preference for the same level of supervision, irrespective of their clinical experience and competence. One study examining pediatric residents compared the ideal frequency of direct supervision with that of direct supervision. The findings revealed that even senior residents sought more frequent and prolonged direct supervision of core skills crucial to independent practice, such as physical examinations and delivery planning [35]. Fig. 3 summarizes these findings.
Discussion
Tremendous efforts have been made to improve entrustment in resident education in order to facilitate the development of independent clinicians. Most studies have explored entrustment in terms of the supervisor or attending person’s perspective, while few have explored the recipients of entrustment—residents. Research has shown that disparities in the perception of entrustment between residents and faculty members can be detrimental to the development of independent physicians. Therefore, this study sought to conduct a comprehensive scoping review of how residents perceive and feel that entrustment affects them.
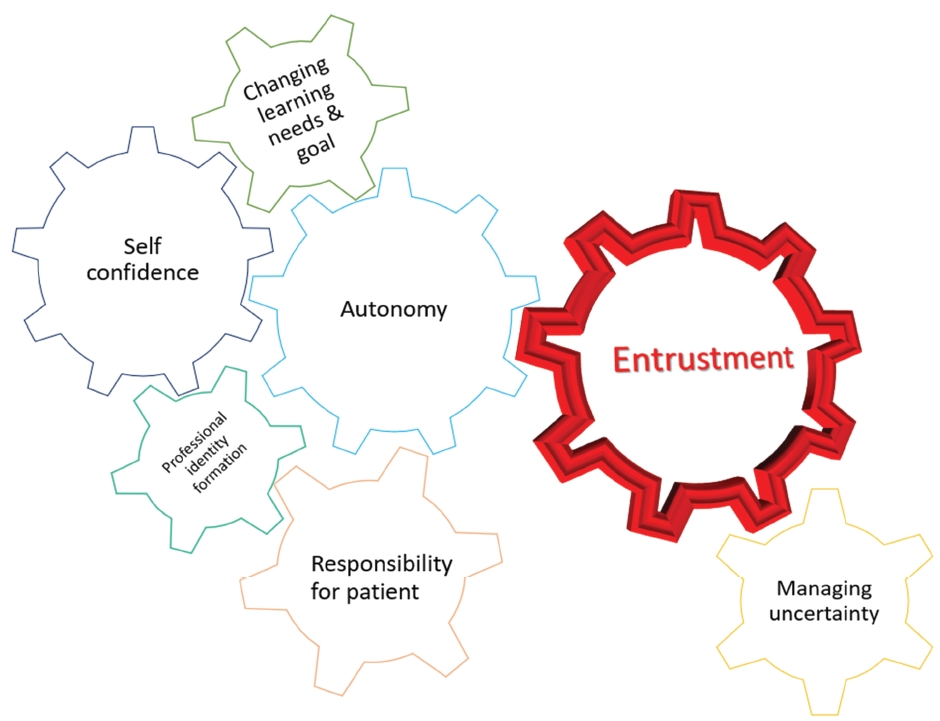
Our review showed that supervisor entrustment significantly influences residents’ clinical performance, including autonomy, self-confidence, responsibility toward patients, changing learning needs and goals, managing uncertainty, and professional identity formation. Various factors, such as supervisors’ attitudes toward residents, promote or hinder residents’ entrustment development. The perceived appropriateness of supervision by residents depended on several factors, including the nature of the tasks entrusted to them, the quality of the supervisor-resident relationship, and the level of teaching effort exerted by the supervisor. Over-supervision and under-supervision were both ultimately detrimental to residents.
The role of autonomy was particularly noteworthy in our findings. Autonomy influences self-confidence, responsibility for patients, and professional identity formation, whereas autonomy and entrustment are intricately connected. Through supervisor entrustment, autonomy was a vital catalyst for residents’ performance, and this process created a feedback loop, further amplifying autonomy and ultimately influencing the formation of a professional identity as a doctor. Moreover, the residents believed that supervisor entrustment influenced their learning to manage uncertainty in medicine. In addition, increasing autonomy and self- confidence by entrustment prompted residents to adapt their learning needs and goal. The authors may interpret the impact of supervisor entrustment on resident’s clinical performance in Fig. 4.
Autonomy refers to the desire to organize experiences and actions subjectively in alignment with one’s self [36]. According to self-determination theory, there is a difference between autonomy and independence [37]. Autonomy does not imply working alone without assistance but rather entails the ability to work based on personal choices without undue pressure. Supervisors must be mindful of this issue when granting autonomy in patient care to students and resident medical trainees. Autonomy in medical training implies that trainees recognize that they are providing patient care out of their own volition [38]. Therefore, supervisors need to be well aware of the disparity between the intended level of autonomy they plan to grant to residents and the level of autonomy expected by residents during the entrustment [39,40]. Effective communication and feedback between residents and supervisors are crucial to bridge this gap. Starting from the initial levels of entrustment, supervisors should regularly share patient care plans with residents and provide timely feedback to foster an understanding of the residents’ learning styles, goals, and developmental levels [39]. Torbeck et al. [40] emphasized that the promotion of autonomy relies heavily on building a trusting relationship between supervisors and residents that matures over time, and advocated for the improvement of the educational paradigm to establish a strong supervisor-learner relationship.
In this review, both self-confidence and responsibility for patients were identified as performances that were significantly shaped by the supervisors’ level of entrustment. However, when looking at the results in depth, researchers primarily considered these performances a secondary gain stemming from an increase in autonomy granted to residents. Additionally, residents’ learning needs and goals shift over time as they gain autonomy and self-confidence, moving from preferring close supervision to desiring more autonomy and independent practice. However, if there are discrepancies between the expected level of autonomy and the actual level of granted autonomy, residents experience demotivation and emotional distress and start focusing on performance over patient-centered care, causing them to question the authenticity of their training. Professional identity formation develops when autonomy, confidence, and responsibility are synergistically enhanced. Given its complicated nature, professional identity formation has been relatively underexplored compared to other key performances. It is necessary to identify the definition and formation process of professional identity from various perspectives and study the influence of supervisor entrustment on the formation process.
The results of this study indicated that learner’s ability to manage uncertainties could be influenced by entrustment decision made by supervisors. Light [41] has noted that residents acquire strategies to navigate medical uncertainty through their training, and the level of entrustment decision impacted resident’s attitudes towards coping with uncertainty [33]. Further detailed research is required to comprehensively understand how residents perceive and respond to medical uncertainty in relation to varying levels of entrustment. This inquiry should elucidate the specific ways in which entrustment levels influence resident recognition and navigation of inherent uncertainties in medical practice.
Through this scoping review, we explored various factors that promote and hinder the development of entrustment. An insightful comparison has been drawn between these identified factors and supervisors’ entrustment decision-making processes in Holzhausen et al. [12]. According to this process, diverse factors influence supervisors’ trust decisions. These encompass the trainee’s characteristics, such as ability, benevolence, and integrity. The characteristics of the supervisors themselves, marked by their experience in supervision, also played a crucial role. The relationship dynamics between the supervisor and learner, characterized by the duration of contact, role assumed by the supervisor, and shared expectations, further swayed the entrustment decisions. Additionally, contextual factors and the characteristics of the task at hand, including its level of complexity, relevance, and frequency of occurrence, crucially influence the decision-making process. These dimensions provide a nuanced understanding of entrustment, showcasing parallels and distinctions in the perceptions of majors and supervisors regarding entrustment development and decision making, respectively.
What is effective supervision, as defined by both supervisors and residents? Comparing our review of appropriate supervision from the residents’ perspective with a previous review from the supervisors’ viewpoint [19], several commonalities and differences emerged. Residents and supervisors shared the following perceptions:
(1) Importance of feedback: Both groups underscored the significance of feedback. Residents perceived supervision as appropriate when they received clear and supportive feedback, especially in challenging situations, while supervisors considered providing feedback fundamental for effective supervision.
(2) Value of autonomy: Residents believed that appropriate supervision should respect their autonomy. Similarly, supervisors implicitly supported autonomy by offering direct guidance without being excessively directive or rigid. They thought that this approach created an environment in which residents could connect theory with practice and engage in collaborative problem-solving.
(3) Mutual trust and respect: For residents, trust was foundational. Appropriate supervision is characterized by mutual trust between supervisors and trainees. From the supervisors’ perspective, effective supervision requires a respectful and empathetic approach toward trainees.
(4) Interpersonal and communication skills: Both residents and supervisors valued effective communication and interpersonal skills. Residents appreciated supervisors who effectively communicated about patient care, shared learning goals, and demonstrated acceptance. Supervisors recognized the necessity of interpersonal and teaching skills for effective supervision.
Despite these shared values and expectations regarding supervision, there were notable differences in the focus and priorities between the two groups. Residents emphasized the importance of aligning tasks with their competency levels and expressed a preference for more frequent supervision of specific core skills, irrespective of their experience. By contrast, supervisors did not explicitly mention task alignment or preferences regarding the level of supervision in their definitions of effective supervision. Recognizing and understanding these commonalities and differences is crucial for fostering supportive and productive supervisory relationships in clinical settings.
A limitation of this study is that we could not examine research results published before the last 10 years. Extending the search period would have allowed us to track changes in the supervisor’s entrustment method and its impact on residents’ perceptions. In addition, some countries may do not use the word entrustment to describe the act of entrusting specific clinical practices to residents during training. Because the main search term for this review included entrustment, literature from countries that did not use the term entrustment was not included in the scoping review. Significantly, this study has enriched our comprehension of how residents perceive supervisor entrustment. However, it is imperative to undertake further research to explore the intricate relationship between autonomy and entrustment.
In conclusion, our review suggests that residents perceived supervisor entrustment as influencing their performance in terms of autonomy, self-confidence, responsibility for patients, shifting learning needs, managing uncertainty, and professional identity formation. Entrustment, as bestowed by supervisors, serves as a catalyst for enhancing autonomy, thereby exerting a significant influence on clinical performance, and fostering the development of a professional identity. However, residents’ views on appropriate supervision revealed both commonalities and differences from supervisors’ perspectives. Further research is needed to bridge the gap between residents’ expectations of autonomy and what they are given, and to explore the intricate relationship between autonomy and entrustment.
Supplementary materials
Supplementary files are available from https://doi.org/10.3946/kjme.2024.286.
Search Keywords
Acknowledgements
None.
Notes
Funding
No financial support was received for this personal view article.
Conflicts of interest
No potential conflicts of interest relevant to this article was reported.
Author contributions
SHS and YML were responsible for the conception and design of the study. SHS and HSK performed the data extraction, analysis, and interpretation. All authors performed the drafting, critical revision, and final approval of the version to be published