The application of augmented reality for improving clinical skills: a scoping review
Article information
Abstract
Augmented reality technology had developed rapidly in recent years and had been applied in many fields, including medical education. Augmented reality had potential to improve students’ knowledge and skills in medical education. This scoping review primarily aims to further elaborate the current studies on the implementation of augmented reality in advancing clinical skills. This study was conducted by utilizing electronic databases such as PubMed, Embase, and Web of Science in June 2022 for articles focusing on the use of augmented reality for improving clinical skills. The Rayyan website was used to screen the articles that met the inclusion criteria, which was the application of augmented reality as a learning method in medical education. Total of 37 articles met the inclusion criteria. These publications suggested that using augmented reality could improve clinical skills. The most researched topics explored were laparoscopic surgery skills and ophthalmology were the most studied topic. The research methods applied in the articles fall into two main categories: randomized control trial (RCT) (29.3%) and non-RCT (70.3%). Augmented reality has the potential to be integrated in medical education, particularly to boost clinical studies. Due to limited databases, however, any further studies on the implementation of augmented reality as a method to enhance skills in medical education need to be conducted.
Introduction
Medical education consists of various methods, primarily on theoretical learning in classrooms and clinical skills in hospitals, where students gain clinical experiences. These learning methods mostly employ the traditional method. Traditional method involves having students come to class multiple times a week. The instructor of the class will often concentrate on instructing, assigning homework, and completing assessments like quizzes, examinations, or projects. The most popular method of instruction is the use of aural and visual aids or media, such as films, demonstrations, or case studies [1].
Rapid innovations and advancement in medical education technology, such as simulation technologies and open-access medical education have occurred recently. The application of augmented reality (AR) as one of simulation technologies in medical education is currently gaining popularity because of its potential to improve the learning qualities [2]. AR can improve the quality of educational settings by providing a life-like experience and interaction of the physical world through the addition of computer-generated sensory input such as sound, video, graphics, or GPS data [2,3]. Previous studies have demonstrated the implementation of AR in multiple settings including medication management and planning, learning tools in medical education and training, simulating objects or organs in surgery for better visualization, improving techniques in rehabilitation for improved outcomes, and many more. As a result, AR system applications will continue to advance and have potential use to facilitate the process of education in healthcare and medical education [2].
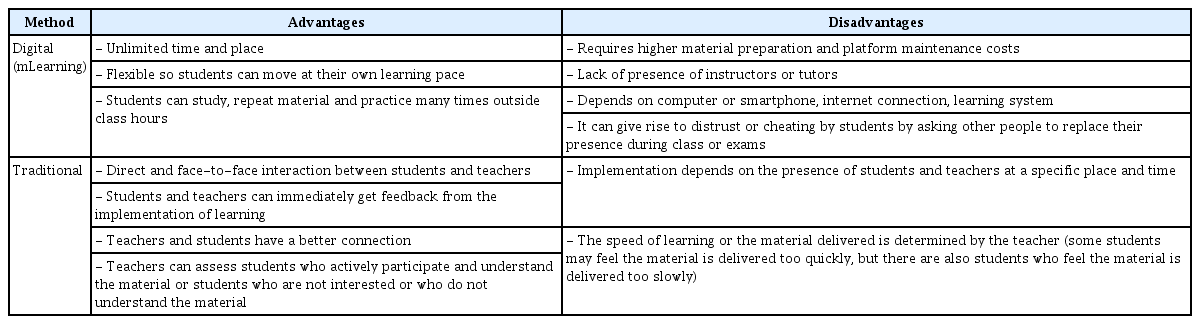
As a result of the use of digital strategies, modern healthcare professional education has undergone a considerable paradigm shift which is now represented in many curricula. Digital learning methods such as using software, videos, gaming, online classes, augmented and virtual reality has proven to have many advantages to improve students’ knowledge and skills. Digital methods are not limited by time or space, and they are flexible, allowing students to learn and practice repeatedly anywhere and anytime. Meanwhile, the disadvantages of this strategy involve higher costs for preparation and platform maintenance, the dependence on the device such as computer or smartphone and Internet connection and the lack of instructors’ presence [1]. The advantages and disadvantages of digital and traditional methods are detailed in Table 1.
Students’ self-confidence is the key factor that influences their success in demonstrating the acquisition of skills. Students want to feel safe during their practices, both for themselves and the patients. Digital learning, for example, AR could be an alternative to improve knowledge and skills in medical students and staffs by providing simulation for trainings [3]. This scoping review mainly purposes to describe the existing research on the use of AR for improving clinical skills.
Methods
1. Information sources
This study conducted by having a scoping review in which the researchers select relevant articles through medical journals and databases such as PubMed, Embase, and Web of Science. A scoping review examines an exploratory research issue and aims to identify important ideas (components), forms of evidence, and research gaps through knowledge synthesis. The titles and abstracts of the papers were examined and analyzed for relevance to the use of AR for enhancing clinical skills using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
2. Eligibility and inclusion criteria
This research involved all articles with the population or participants who were provided intervention using AR technology to compare the technology with the existing traditional methods to improve their clinical skills. This study used randomized control trial and experimental studies which compared two methods of study using AR and the traditional methods.
1) Exclusion criteria
Non-English language articles; discussion, book chapters, proceedings, and dissertations/thesis were excluded.
2) Databases
From the inception of the research to June 2022, the researchers had searched three databases; PubMed, Embase, and Web of Science.
3) Search strategy
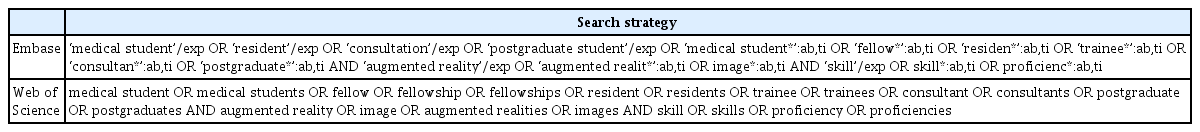
This research employed a combination of Medical Subject Headings (MeSH) and free-text search terms for AR and skills as described in Table 2.
This study used Rayyan Intelligent Systematic Review (https://www.rayyan.ai/), a free online application that assisted systematic review methodology and meta-analysis projects, to filter the articles that met the inclusion criteria. This application allows user to search the existing citation records such as title, abstract, and author.
3. Data extraction and analysis
The extracted data obtained from various literatures were analyzed using both qualitative and descriptive method. The researchers retrieved descriptive data concerning year of publication, type of artificial intelligence used in the study, number of subjects, outcome of study, and parameter/assessment tool as well as took note on the results of the studies. In the analysis stage, all data were meticulously analyzed using Braun and Clarke’s qualitative thematic analysis, a widely used method in scoping reviews. In addition, this review applied a comprehensive thematic representation of certain research areas, and artificial intelligence application to improve skills of medical students were carefully selected. Familiarization of data set included type of study, type of AR, and outcome/parameter of assessment. The authors discussed theme review, data, and collation and excluded articles with had little engagement with the key issue (AR and skill improvement) and those that mentioned the bias issues.
Results
1. Synthesis of results
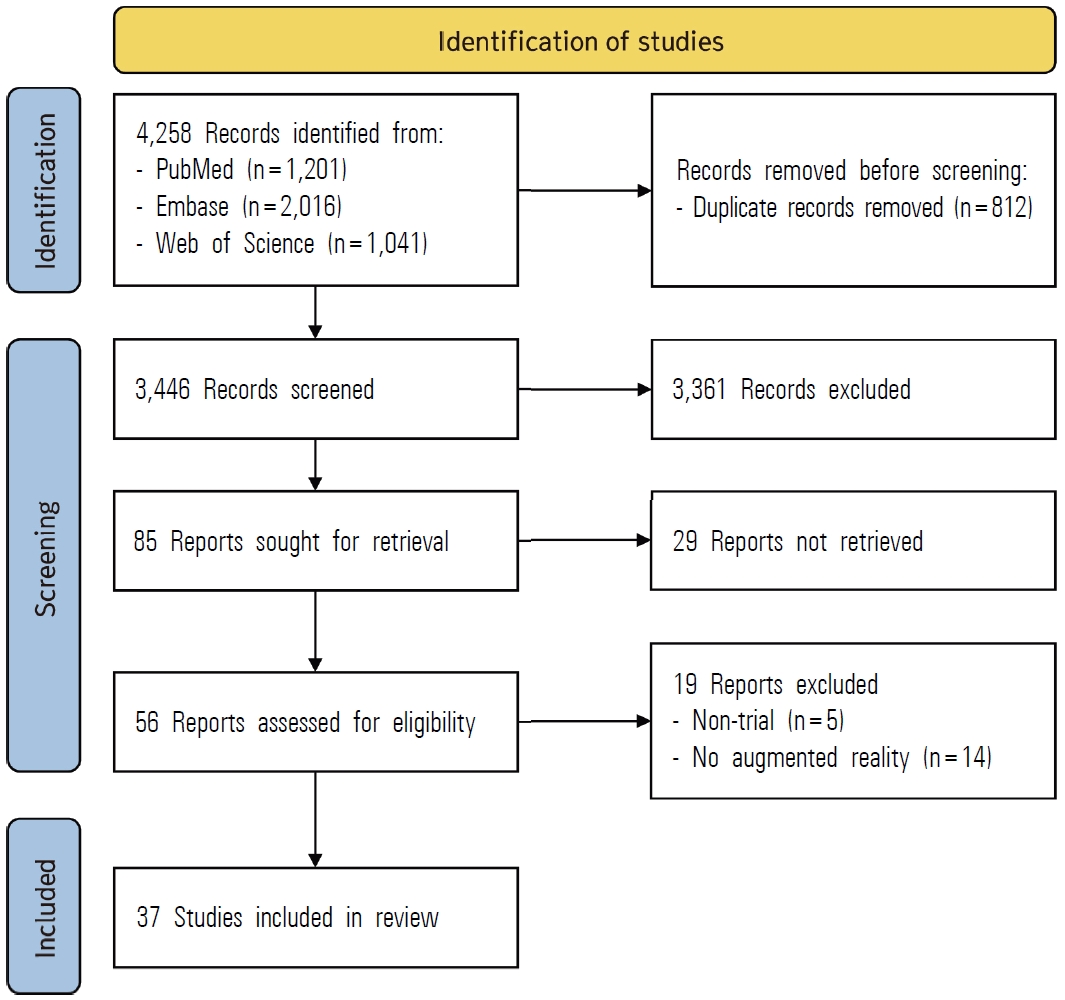
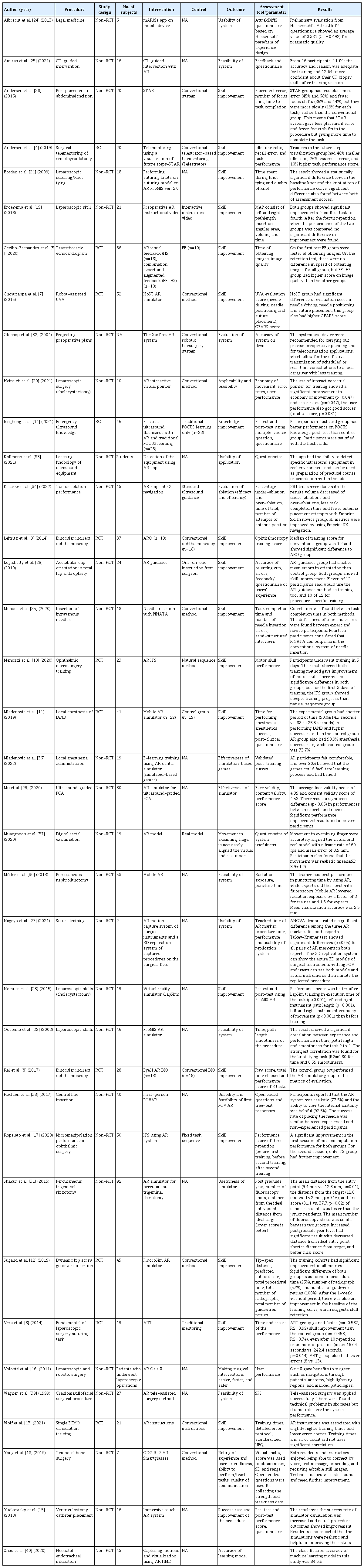
The initial search yielded a total of 4,258 entries. After the process of filtering, eliminating duplicates, screening, and excluding them based on titles and abstracts, 85 publications were reviewed in the study. A total of 37 articles were then selected for the full-review study. The PRISMA flow diagram of the study selection is presented in Fig. 1. This research focused on several countries: the United States (n=10), Canada (n=4), the United Kingdom (n=4), Germany (n=4), Switzerland (n=4), Netherlands (n=3), Serbia (n=2), Austria (n=2), Japan (n=2), Portugal (n=1), and Thailand (n=1). All study’s characteristics included in this study were described in Table 3 [4-40].
2. Randomized control trial articles
The previous studies used randomized control trials (RCTs) to investigate the application of AR. Eleven publications (29,7%) of 37 publications reviewed in this study employed RCT as the research method. These publications originated from a variety of medical science fields, the majority of which dealt with surgery. Ten articles investigated skill enhancement after adopting AR as a novel learning technique. By giving participants a new method of mentoring or teaching, AR system was applied to improve skills in cricothyroidotomy [4], transthoracic echocardiogram [5], and laparoscopic suturing task [6], Robotic system, simulator, and instructions using AR were also used in urethrovesical anastomosis [7], ophthalmoscopy and ophthalmic microsurgery [8-10], local anesthesia of inferior alveolar nerve block [11], dynamic hip screw guidewire [12], and single extracorporeal membrane oxygenation (ECMO) cannulation [13]. One study used AR with flashcards to improve emergency ultrasonography knowledge [14]. Ten articles found that the AR intervention group outperformed the traditional approach control group.
3. Non-randomized control trial articles
There were 26 articles (70,3%) of 37 articles examined in this study employed non RCT study methods. Besides, 11 articles concentrated on skill improvement, and all of the studies focused on improvement. AR is essential to help medical practitioners do laparoscopic suturing, knot-tying training, and better visualization for digital rectal examination. AR has been used in tele-mentoring to assist students in achieving better skills in port placement and abdominal incision. The implementation of AR to provide learning assisting is considered advantageous for acetabular cup orientation in total hip arthroplasty. The growing popularity of AR in the medical field aids numerous departments in developing their skills and simplifying their work. The non-RCT articled reviewed stated that Immersive Touch simulator can increase success rate of ventriculostomy catheter placement [15]. OsiriX assists surgeons in navigating patients’ anatomy [16]. The improvement of clinical skills is possible using intelligent tutoring system for micromanipulation in ophthalmic surgery [17]. Despite requiring improvement, ODG (Osterhout Design Group) R-7 Smartglasses (https://www.osterhoutgroup.com/products-r7HL/) is used in temporal bone surgery experience [18], Meanwhile, other 15 articles had investigated the application of AR in skill improvement, with an emphasis on the system’s usability or feasibility.
4. Augmented reality in laparoscopic surgery skills
Minimally invasive surgery technique such as using laparoscopy for surgery has become widespread in various areas of surgery. This technique has numerous benefits including a lower risk of infection, less surgical stress and complications, and a shorter hospital stay and recovery time. The application of AR is able to facilitate the process of learning and training of laparoscopic surgery skills. The majority of articles in this review investigated the utilization of AR to enhance laparoscopic surgical skills. One study examined how instructional video scheduling has affected learning curves for laparoscopic skill training. The participants first received a course on the basic skills on virtual reality simulator before divided into two groups of instructional videos either preoperatively or intraoperatively. Both groups improved their laparoscopic skills, with no significant differences [19]. Another study looked on the use of optical see-through AR to view an interactive virtual pointer on the laparoscopy. The participants would be separated into two groups: HoloPointer and standard. The results revealed that the HoloPointer group outperformed the regular group. The HoloPointer group also exhibited a reduction in mistakes and increased movement economy [20]. The ProMIS Augmented Reality laparoscopic simulator was investigated to improve laparoscopic suturing abilities and found a substantial difference in the participants’ performance curves and metrics [21,22]. Nineteen participants completed a 6-week training program utilizing a virtual reality simulator (LapSim) and were evaluated using an AR simulator (ProMIS) for cholecystectomy performance, demonstrating improvement in surgical skills [23]. The use of AR telementoring for laparoscopic surgery intracorporeal suturing task shown faster skill development and fewer failures than standard learning methods [6].
5. Augmented reality in ophthalmology
In order to establish a diagnosis, indirect ophthalmoscopy was a necessary examination in ophthalmology. Training for these skills requires trial and error, and numerous approaches, including fundus dummies, have been devised. Augmented reality ophthalmoscopy (ARO) was created to assist students in learning and practicing binocular indirect ophthalmoscopy. The ARO group improved their ophthalmoscopy skills faster than the traditional group [9]. EyeSI, which was comparable to ARO, an AR binocular indirect ophthalmoscopy simulator developed and investigated in Canada to be contrasted with traditional teaching methods, was developed and studied. The EyeSI group outperformed the typical group and improved significantly [8]. Students are trained for skill improvement in microsurgical operations using AR. One study looked into the use of AR to improve motor abilities and intelligent tutoring systems to improve training efficiency. The results demonstrated that adopting AR as a training tool improved skill. Students’ performance improved with both intelligent tutoring system and natural sequential steps or classic training [10,17].
Discussion
1. Principal findings
AR is a novel technology that has a variety of applications that are constantly being developed. AR is a technology that combines two-dimensional or three-dimensional virtual objects into a three-dimensional real environment, then projects these virtual objects in real time. One of the elements contributing to its growing popularity is the ability to observe and interact with digital objects without having to turn away from the real world to view the monitor displaying the appropriate medical imaging [41]. The difference between AR and virtual reality are AR using real-world setting and enhances both virtual and real world, users can control their presence in real world and AR can be accessed with smartphone while virtual reality is completely virtual, controlled by the system and required headset device. This scoping analysis was carried out to describe the existing research on the use of AR in improving medical practitioners’ clinical abilities. This scoping review discovered 37 papers that met the criteria. More than 80% of the publications in this review stated that using AR could improve clinical skills. AR is able to outperform the conventional methods of learning by providing more improvement of students’ knowledge and skills.
A comparison of the effects of mobile AR learning and textbook learning on medical students revealed that the mobile AR group improved their knowledge more than the control group [24]. These findings were also seen in the publications we examined for this investigation. They discovered that AR improved and increased the effectiveness of learning.
Because of the disparities in what medical students learned in school and in clinical settings, it was discovered that surgery and interventional procedures received more attention in the development of new digital learning tools. Students’ knowledge and abilities will not improve until they practice them. Chowriappa et al. [7] used an RCT to compare the use of AR, namely hand-on surgical training, and traditional approaches in skills training for robot-assisted urethrovesical anastomosis. The results demonstrated that the AR training increased students’ skills [7]. Other studies focusing on skill improvement in surgery and the interventional procedure category were computed tomography (CT)-guided intervention [25], port placement and abdomen incision [26], basic and laparoscopic skills and suturing [16,22,27], cholecystectomy [20,23], total hip arthroplasty [28], percutaneous renal access and nephrolithotomy [29,30], percutaneous rhizotomy [31], ECMO cannulation, and transthoracic echocardiogram [5,13]. It is found that AR is used to improve language learning, mechanical skills, and spatial abilities in addition to clinical skills.
Each AR application or device has its unique user interface and benefits that may or may not be applicable in all circumstances. The standard approaches evaluated still increase clinical skill learning, but the AR groups demonstrated greater improvement. Previous research has demonstrated the advantages of using AR in medical education, such as minimizing radiation exposure. Park et al. [42] investigated how the use of AR could increase procedural efficiency in terms of process time, puncture, and radiation exposure for CT-guided intervention. Park et al. [42] discovered that utilizing AR in CT-guided intervention reduced the mean CT dose index from 28.7 to 16.9 mGy.
AR also shows its effectiveness in improving surgical skills through telementoring, which offers experts in faraway locations real-time guidance on surgical operations. This can be a potential to use AR in the future as a tool for supervision and skill development. For surgical novices, expert supervision is crucial, and AR telementoring may provide more flexibility and efficiency than traditional “direct” supervision, which in certain cases might be demanding and ineffective. Also, considering that objective performance indicators may be monitored utilizing AR platforms in a simulated or, ideally, real-life operational environment to assess technical ability, the function of AR as an evaluation tool is worth taking into account [43,44].
AR applications are most successful in motivating users for training and knowledge transmission. It serves as a tool to provide interactive experiences and makes users feel comfortable with decisions and supported while doing skills or activities. However, technological concern such as latencies, eyesight, perception, a lack of ergonomic gear, location and accuracy failures, illumination occlusions, and other technical issues remain as the disadvantages of this digital method of learning and needed to be solved [45]. As this technology develops, further research will be required to assess various modalities that AR may be applied to. To be effective, future AR devices would also need to be able to interface and link up with other medical equipment, such emergency medical record systems, ultrasound machines, and vital monitors. It will be necessary to create software standards for this [2].
2. Strength and limitations
This review may provide insight into the potential application of AR as a learning tool in medical education and training. It also could inform the application of AR across various areas or departments in medical fields. The majority of articles on the development of AR technology highlight industrialized countries and significant medical education centers. AR is still considered a novel and expensive technology in medical sectors. Another limitation is that the included studies only discussed small-scale AR implementations and used a variety of AR platforms. For further research on the use of AR to improve students' skills, the researchers advise using and applying AR by using an application (mobile or PC) or online that provides AR simulation, if access and expense are limited.
Conclusion
AR has the potential to be integrated in medical education, particularly to boost clinical studies. Due to limited databases, however, any further studies on the implementation of AR as a method to enhance skills in medical education need to be conducted.
Acknowledgements
None.
Notes
Funding
None.
Conflicts of interest
No potential conflict of interestrelevant to this article was reported.
Author contributions
Conception or design of the work: MM, DCR, DS, NA; data collection: MM; data analysis: MM, DCR, DS, NA; data interpretation: MM, DCR, DS, NA, MAZ; drafting the article: MM; critical revision of the article: MM, DCR, DS, NA, MAZ; and final approval of the version to be published: DCR, DS, NA.